Situation at a glance
Description of the situation
As of 20 November 2025, 33 laboratory tests have been conducted, of which six confirmed cases, including three deaths, have been reported. Of the six confirmed cases, three are currently alive and on treatment. In addition to the lab-confirmed cases, a further three epidemiologically linked cases could not be tested; all three are deceased and recorded as probable cases. A total of 206 contacts have been identified, and contacts are under active follow-up. The number of contacts will continue to change as the response evolves.
Clinically, patients have presented with high-grade fever, headache, vomiting, abdominal pain, and watery or bloody diarrhoea. Haemorrhagic manifestations, including nose bleeding and vomiting blood were observed in five cases, consistent with multi-organ failure.
As this is the first time Ethiopia is reporting MVD, WHO recommends that samples be shared with a reference laboratory for inter-laboratory comparison.
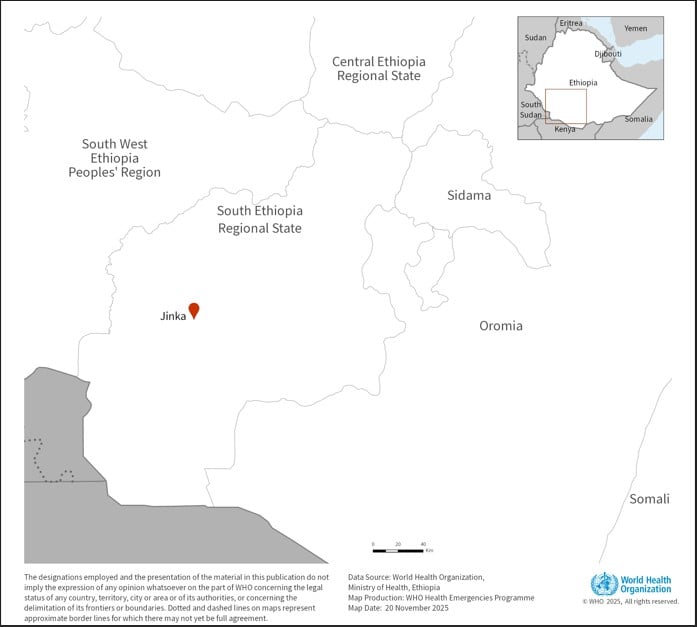
Figure 1: Map of Ethiopia showing location of Jinka town
Epidemiology
Marburg virus disease (MVD) is a severe hemorrhagic fever caused by either of two closely related viruses, Marburg virus and Ravn virus, which are closely related to the Ebola viruses. MVD has a high case fatality rate, ranging from 24% to 88% from previous outbreaks The case fatality rate can be lowered with good and early patient care. The virus is initially transmitted to humans from fruit bats (Rousettus aegyptiacus) and then spreads among people through direct contact with bodily fluids, contaminated surfaces, or infected materials. Healthcare workers, caregivers, and individuals involved in burial practices are particularly at risk when infection prevention and control measures are not in place.
MVD symptoms typically begin abruptly after an incubation period of two to 21 days and include high fever, severe headache, malaise, muscle aches, and progressive gastrointestinal symptoms such as diarrhea and vomiting. In severe cases, patients may experience bleeding from multiple sites and die from shock and organ failure within a week of symptom onset.
There are no approved treatment or vaccines for MVD, although supportive treatment and early supportive care improves survival. Some candidate vaccines and therapeutics are currently under investigation.
Nineteen outbreaks of MVD have previously been reported globally. The most recent outbreak was reported from the Republic of Tanzania between January and March 2025. Additional countries that have reported outbreaks of MVD in the African Region include Angola, the Democratic Republic of the Congo, Equatorial Guinea, Ghana, Guinea, Kenya, Rwanda, South Africa, and Uganda.
Public health response
Local and national health authorities in Ethiopia have implemented the following public health measures:
- A National Taskforce has been established at the Ministry of Health to provide strategic guidance, make decisions and mobilize resources.
- A costed national three-month response plan has been developed and launched by the MoH/EPHI.
- The MoH is regularly providing information on the MVD outbreak to the general public and partners.
- Emergency Operational Centres (EOCs) have been activated at national and regional levels, with incident management structures established to coordinate the response. Daily coordination meetings are ongoing at the national and subnational EOCs.
- The Ministry of Health, in collaboration with EPHI and regional health offices, is conducting integrated surveillance and response activities.
- Community surveillance, contact tracing, house-to-house visits, and medical service delivery are being enhanced.
- Two hospitals have been designated as treatment centres, with dedicated health workers deployed to manage cases.
- Field assessments are being conducted by a rapid response team (RRT). One RRT was deployed to Jinka to conduct contact tracing and epidemiological investigation while a second team is strengthening infection prevention and control (IPC) in health facilities managing suspected cases.
- Risk Communication and Community Engagement (RCCE) teams are disseminating MVD prevention messages, developing activity plans for targeted interventions, monitoring social media to address misinformation, and assessing trusted communication channels to enhance public awareness.
WHO risk assessment
This is the first confirmed MVD outbreak in Ethiopia. The public health risk posed by the MVD outbreak is assessed as high at the national level due to several concerning factors:
- The outbreak involves six laboratory-confirmed cases; there have been a total of six deaths and there are three confirmed cases under treatment.
- All deaths involved unsupervised burials, posing a risk of potential additional community transmission.
- The presence of healthcare workers among the confirmed cases suggests potential occupational exposure risks within health facilities.
- Although investigations are ongoing, information on the source of the outbreak, geographical extent and epidemiology is limited.
Although no international transmission has been confirmed to date, the potential risk for spread remains. The affected area, Jinka, while distant from Ethiopia’s capital or major international airports, is connected by road transportation networks, including to neighbouring Kenya and South Sudan. Therefore, the public health risk posed by this event is assessed as moderate at the regional level. It is considered low at the global level.
WHO advice
Human-to-human transmission of Marburg virus is primarily associated with direct contact with the blood and/or other bodily fluids of infected people. Strengthening and reinforcing IPC measures is essential to prevent further transmission and reduce the likelihood of amplification.
WHO advises the following risk reduction measures to be taken as an effective way to reduce MVD transmission to control the outbreak.
Prevention: Protective measures individuals should take to reduce human exposure to the virus include:
- Reduce the risk of human-to-human transmission in the community arising from direct or close contact with infected patients, particularly with their body fluids including blood, feces and vomit. Close physical contact with MVD patients should be avoided.
- Persons with symptoms compatible with MVD should immediately seek care in health facilities, and patients suspected or confirmed to have MVD should be isolated in a designated treatment centre for early care and to avoid transmission at home.
- Community and family members should avoid caring for symptomatic individuals at home and avoid touching bodies of people deceased with MVD symptoms. They should avoid touching other potentially contaminated items and surfaces.
- Reduce the risk of bat-to-human transmission arising from prolonged exposure to mines, caves or dwellings inhabited by fruit bat colonies. During work or research activities or tourist visits in mines or caves inhabited by fruit bat colonies, people should wear gloves and other appropriate protective clothing (including masks). During outbreaks, all animal products (blood and meat) should be thoroughly cooked before consumption.
Coordination: Multisectoral coordination and pillar meetings at all levels and sharing of detailed situation reports is encouraged. Involvement of different stakeholders and partners in preparedness and response activities is also encouraged. To ensure an effective and sustained response, resource mobilization efforts within the government and with partners are recommended.
Risk communication and community engagement: Raising public awareness and engaging with communities are important for successfully controlling MVD outbreaks. This includes raising awareness of symptoms, risk factors for infection, protective measures and the importance of seeking immediate care at a health facility. Sensitive and supportive information about safe and dignified burials is also crucial. This awareness should be increased through targeted campaigns and direct work with communities. Special attention should be given to high-risk groups, such as traditional healers, clergy, and community leaders, who may inadvertently facilitate disease spread, and who are important sources of information for the community. Misinformation and rumours should be addressed to foster trust and promote early symptom reporting.
Surveillance: Active case detection, contact tracing, and alert management across affected and neighbouring regions should be intensified. Community-based surveillance systems should be strengthened to promptly identify and report new cases, particularly in high-risk areas. Close monitoring of healthcare workers, family members and individuals who have had contact with suspected cases or other high-exposure settings should be ensured. Surveillance capacities should also be intensified at relevant points of entry and borders to reduce the risk of further spread, including internationally.
Infection prevention and control (IPC) measures:
- Critical infection prevention and control measures should be implemented and/or strengthened in all health care facilities, per WHO’s Infection prevention and control guideline for Ebola and Marburg disease, which highlighted the importance of the rapid implementation of the IPC ring approach, including but not limited to IPC rapid assessment, decontamination of health facilities and households and early detection and identification of the cases through the screening and isolation of the suspected cases to minimize the transmission risk. Patients meeting the case definition for suspected MVD should be treated with appropriate precautions for MVD, regardless of whether the clinical suspicion suggests a more common ailment with similar symptoms, such as malaria.
- Health workers caring for patients with confirmed or suspected MVD should apply transmission-based precautions in addition to standard precautions, including appropriate use of personal protective equipment (PPE) and hand hygiene according to the WHO 5 moments, to avoid contact with patient’s blood and other body fluids and with contaminated surfaces and objects. Waste generated in healthcare facilities must be safely segregated, safely collected, transported, stored, treated and finally disposed. Follow the national guidelines, rules and regulations for safe waste disposal or follow the WHO’s guidelines on safe waste management.
- Patient-care activities should be undertaken in a clean and hygienic environment that facilitates practices related to the prevention and control of health-care-associated infections (HAIs) as outlined in Essential environmental health standards in health care. Safe water, adequate sanitation and hygiene infrastructure and services should be provided in healthcare facilities. For details on recommendations and improvement, follow the WASH FIT implementation Package.
Laboratory testing: The processing and analysis of samples should be expedited, with results promptly shared with responders and clinicians to guide patient management, containment strategies and broader response efforts. This includes genomic sequencing on positive samples. International referral of samples to a regional reference laboratory should be considered for inter-laboratory comparison. Laboratory workers handling specimens from patients suspected or confirmed to be infected with MARV should receive refresher training on laboratory biosafety; this includes taking appropriate precautions when drawing blood for a malaria rapid diagnostic test or other test not specific for MARV.
Evaluation of candidate medical countermeasures: There are no licensed vaccines or therapeutics against MVD. Several candidate vaccines are in the pipeline and outbreaks offer an opportunity to assess their efficacy and safety. There are protocols available and a network of experts in filoviruses ready to support national researchers.
Safe and dignified burials: Safe and dignified burial protocols should be implemented for persons who have died to minimize community exposure. Additional training and equipment for healthcare workers and burial teams should be provided to ensure safe management of MVD-related fatalities. Thorough community engagement is required to ensure that affected communities are empowered to adhere to the protocols.
Case management and mental health and psychosocial support: Designated treatment centers should ensure adequate level of care for confirmed patients to improve the chance of survival. Isolation and treatment facilities should be adequately equipped to ensure the safety and efficacy of patient care, while simultaneously preventing the spread of the disease. Supportive care such as rehydration, symptom management, and psychological support for patients and their families is essential to improving survival rates and mitigating the outbreak's impact.
Border health and cross-border coordination: Surveillance capacities should be strengthened at relevant at-risk points of entry, onboard conveyances, and in border regions to prevent further spread, including internationally. Cases, contacts and individuals in affected areas who present signs and symptoms compatible with case definition should be advised not to travel, in line with WHO’s border health and points of entry technical guidance for filovirus disease outbreaks. Collaboration with neighbouring countries should be enhanced to harmonize reporting mechanisms, conduct joint investigations, and share critical data in real-time. Countries at-risk of potential spread should enhance readiness activities to enable early case detection, isolation and treatment.
Based on the current risk assessment, WHO advises against any travel and trade restrictions with Ethiopia.
Further information
- An introduction to the Marburg virus vaccine consortium, MARVAC | PLOS Pathogens [Internet]. [cited 2025 Nov 19]. Available from: https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1010805
- Bat‐borne viruses in Africa: a critical review - Markotter - 2020 - Journal of Zoology - Wiley Online Library [Internet]. [cited 2025 Nov 19]. Available from: https://zslpublications.onlinelibrary.wiley.com/doi/10.1111/jzo.12769
- Building research readiness for a future filovirus outbreak, Workshop February 20 - 22, 2024, Uganda [Internet]. [cited 2025 Nov 19]. Available from: https://www.who.int/news-room/events/detail/2024/02/20/default-calendar/building-research-readiness-for-a-future-filovirus-outbreak-workshop-february-20-22-2024-uganda
- Diagnostic testing for Ebola and Marburg virus diseases: interim guidance, 20 December 2024 [Internet]. [cited 2025 Nov 19]. Available from: https://www.who.int/publications/i/item/B09221
- My Mooc [Internet]. [cited 2025 Nov 19]. Ebola and Marburg diseases screening and treatment center design. Available from: https://www.my-mooc.com:443/en/mooc/ebola-and-marburg-diseases-screening-and-treatment-center-design-openwho-org-b254d40e-8763-4fce-9847-5bfea7afa8c8
- Ebola and Marburg treatment centres [Internet]. World Health Organization; 2024 [cited 2025 Nov 19]. Available from: https://www.who.int/publications/b/73031
- Ethiopia reports suspected viral haemorrhagic fever outbreak | WHO | Regional Office for Africa [Internet]. 2025 [cited 2025 Nov 19]. Available from: https://www.afro.who.int/news/ethiopia-suspected-viral-haemorrhagic-fever-outbreak
- Facebook [Internet]. [cited 2025 Nov 19]. Available from: https://www.facebook.com/photo?fbid=1248868497275378&set=a.288278136667757
- Hand hygiene technical reference manual: to be used by health-care workers, trainers and observers of hand hygiene practices [Internet]. [cited 2025 Nov 19]. Available from: https://www.who.int/publications/i/item/9789241598606
- Infection prevention and control guideline for Ebola and Marburg disease, August 2023 [Internet]. [cited 2025 Nov 19]. Available from: https://www.who.int/publications/i/item/WHO-WPE-CRS-HCR-2023.1
- Laboratory biosafety manual, 4th edition [Internet]. [cited 2025 Nov 19]. Available from: https://www.who.int/publications/i/item/9789240011311
- Marburg virus disease [Internet]. [cited 2025 Nov 19]. Available from: https://www.who.int/news-room/fact-sheets/detail/marburg-virus-disease
- Marburg virus disease [Internet]. [cited 2025 Nov 19]. Available from: https://www.who.int/news-room/questions-and-answers/item/marburg-virus-disease
- Marburg virus disease - United Republic of Tanzania [Internet]. [cited 2025 Nov 19]. Available from: https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON471
- Marburg virus therapeutics landscape [Internet]. [cited 2025 Nov 19]. Available from: https://www.who.int/publications/m/item/marburg-virus-therapeutics-landscape
- Marburg virus vaccine landscape [Internet]. [cited 2025 Nov 19]. Available from: https://www.who.int/publications/m/item/marburg-virus-vaccine-landscape
- Standard precautions for the prevention and control of infections: aide-memoire [Internet]. [cited 2025 Nov 19]. Available from: https://www.who.int/publications/i/item/WHO-UHL-IHS-IPC-2022.1
- Steps to put on personal protective equipment (PPE) for Ebola/Marburg disease: Coverall [Internet]. [cited 2025 Nov 19]. Available from: https://www.who.int/multi-media/details/steps-to-put-on-ppe-for-ebola-marburg-disease-coverall
- Steps to put on personal protective equipment (PPE) for Ebola/Marburg disease: Gown and headcover [Internet]. [cited 2025 Nov 19]. Available from: https://www.who.int/multi-media/details/steps-to-put-on-ppe-for-ebola-marburg-disease-gown-and-headcover
- Steps to remove personal protective equipment (PPE) for Ebola/Marburg disease: Coverall [Internet]. [cited 2025 Nov 19]. Available from: https://www.who.int/multi-media/details/steps-to-remove-ppe-for-ebola-marburg-disease-coverall
- Steps to remove personal protective equipment (PPE) for Ebola/Marburg disease: Gown and headcover [Internet]. [cited 2025 Nov 19]. Available from: https://www.who.int/multi-media/details/steps-to-remove-ppe-for-ebola-marburg-disease-gown-and-headcover
- This document describes a long-term global strategy for filovirus research and monitoring. [Internet]. [cited 2025 Nov 19]. Available from: https://www.who.int/publications/m/item/a-who-strategic-research-agenda-for-filovirus-research-and-monitoring-----(who-afirm)
- Transmission-based precautions for the prevention and control of infections: aide-memoire [Internet]. [cited 2025 Nov 19]. Available from: https://www.who.int/publications/i/item/WHO-UHL-IHS-IPC-2022.2
- Viral Haemorrhagic Fever | WHO | Regional Office for Africa [Internet]. 2025 [cited 2025 Nov 19]. Available from: https://www.afro.who.int/health-topics/viral-haemorrhagic-fever
- WHO Technical Advisory Group – candidate vaccine prioritization. Summary of the evaluations and recommendations on the four Marburg vaccines [Internet]. [cited 2025 Nov 19]. Available from: https://www.who.int/publications/m/item/who-technical-advisory-group---candidate-vaccine-prioritization.--summary-of-the-evaluations-and-recommendations-on-the-four-marburg-vaccines
Citable reference: World Health Organization (21 November 2025). Disease Outbreak News; Marburg virus disease in Ethiopia. Available at: https://www/who.int/emergencies/disease-outbreak-news/item/2025-DON585
