Situation at a glance
Description of the situation
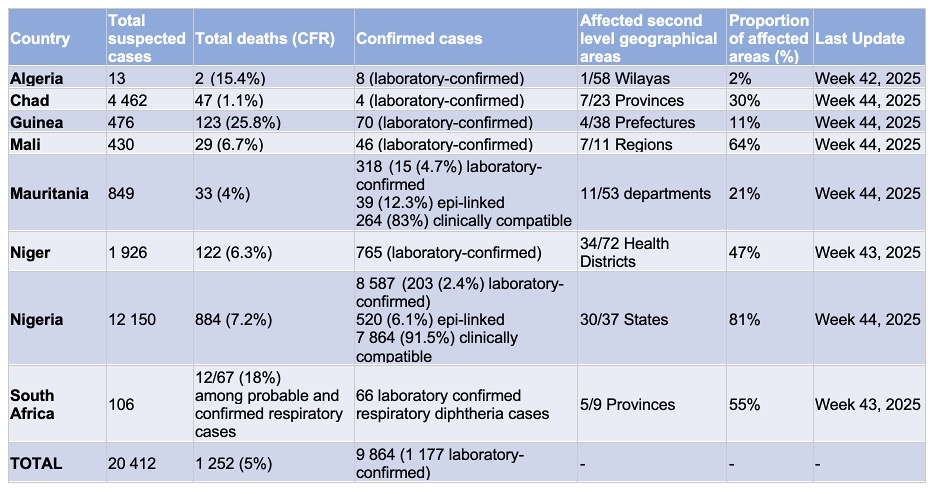
In 2025, from 1 January to 2 November, a total of 20 412 suspected diphtheria cases, including 1 252 deaths (an average case fatality ratio [CFR] – 6.1 %) have been reported across eight Member States in the WHO African Region (Algeria, Chad, Guinea, Mali, Mauritania, Niger, Nigeria, and South Africa). Of these suspected cases, 9 864 (48.3%) cases have been confirmed through laboratory testing, epidemiological linkage, or clinical diagnosis. Laboratory confirmation was conducted for 5.7% (n = 1 177) of the suspected cases.
Women, children aged 5–18 years, and young adults under 30 years are the most affected, confirming that the immunity gap extends well beyond early childhood. The situation has further deteriorated in Mali, Mauritania, and Niger, in recent weeks, with increasing case numbers and geographic spread of the outbreaks reported in these countries.
The resurgence of diphtheria across multiple countries in the WHO African Region constitutes a serious public health concern which led to its grading as a grade 2 emergency under the Emergency Response Framework of WHO. Timely case detection, coordinated response, and clinical management remain critical to limiting transmission and reducing the high fatality rates observed in recent outbreaks. However, response efforts are being hampered by a global shortage of DAT and limited laboratory diagnostic capacity.
Effective outbreak control requires comprehensive, multi-sectoral action across all response pillars including emergency coordination, laboratory confirmation, enhanced surveillance and case finding, clinical management with life-saving DAT and appropriate antibiotics (in accordance with WHO guidelines), infection prevention and control (IPC). Sustained vaccination efforts, coupled with risk communication and community engagement (RCCE) are essential to interrupt transmission and protect high-risk populations. In addition, preventing the recurrence of diphtheria outbreaks in the African Region will require strengthened health systems, particularly through robust routine immunization coverage.
Summary of individual country situations from 1 January to 2 November 2025
Algeria
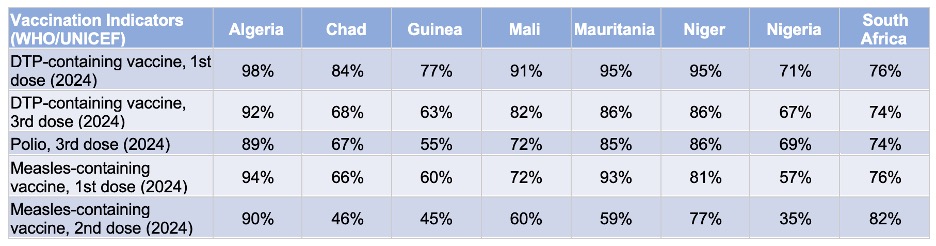
Algeria reported a diphtheria outbreak in October 2025 in Skikda province, with 13 suspected cases and two deaths (CFR 15%). Eight of the suspected cases were laboratory-confirmed, and none of the confirmed cases had received diphtheria vaccination. The outbreak affected both children and adults, with males accounting for 62.5% of confirmed cases. A previous outbreak in southern Algeria, reported in 2024, involved over 900 suspected cases and 119 deaths (CFR 13%). According to WHO/UNICEF estimates of national immunization coverage (WUENIC) for 2024, Algeria has high national immunization coverage (98% for the first Diphtheria-Tetanus toxoid-Pertussis [DTP] dose and 92% for the third), however geopolitical instability in neighboring countries has led to mass displacement into southern Algeria, where vaccination coverage among refugees is low. The lack of data since May 2025 and limited information sharing are key challenges to assessing the full scope of the outbreak.
Chad
From 1 January to 2 November 2025, Chad reported 4 462 suspected diphtheria cases and 47 deaths (CFR 1.1%), with only four laboratory-confirmed cases. The significant amount of suspected diphtheria cases compared to the limited number of laboratory-confirmed cases highlights the challenge in the country to obtain a laboratory-confirmed diagnosis. The outbreak affects 27 out of 215 health districts across 7 of 23 provincial health delegations, with active transmission ongoing in three regions. Most cases are among children aged 3–13 years, and vaccination status is unknown for the vast majority. Chad faces a complex humanitarian crisis marked by conflict, displacement, and food insecurity. The country hosts over 1.4 million refugees, including more than 870 000 Sudanese refugees and 300 000 Chadian returnees. The health system is overwhelmed, and multiple infectious disease outbreaks, including yellow fever, measles, cholera, and hepatitis E, are occurring simultaneously. WHO, UNICEF, and MSF are supporting response efforts, but challenges include delayed reporting, insufficient case management kits, and logistical constraints. A request has been submitted to Gavi for vaccine supply and operational funding for mass immunization campaigns. According to WUENIC, the DTP coverage in 2024 was 84% for the first dose and 68% for the third dose.
Guinea
Guinea has experienced a resurgence of diphtheria since June 2025, with 476 suspected cases and 123 deaths. The CFR among the suspected cases is 25.8%, the highest among affected countries. The outbreak has affected four of 38 prefectures (11%), with human-to-human transmission concentrated in the Kankan region, particularly in Siguiri district, which accounts for over 80% of reported cases and fatalities. Laboratory confirmation remains limited, with only 70 cases confirmed. The outbreak follows a major event in 2023 that affected multiple regions and led to over 4 500 suspected cases. Guinea’s response is hampered by delayed presentation to health facilities, and insufficient resources for clinical management and community engagement. The outbreak is occurring in gold mining areas with high population mobility, increasing transmission risk. According to WUENIC in Guinea for 2024, the immunization coverage remains low (77% for the first DTP dose and 63% for the third), and urgent needs include DAT supply, improved clinical pathways, and expanded vaccination efforts.
Mali
From 1 January to 2 November 2025, Mali has reported 430 suspected diphtheria cases and 29 deaths (CFR 6.7%), with 46 laboratory-confirmed cases. The outbreak has affected seven out of 11 regions (64%), including the capital city Bamako, with the number of affected districts increasing from three to 30 out of 75 in less than six weeks, representing a rapid geographic expansion. Mali is experiencing a complex humanitarian crisis driven by conflict, climate related disruptions, and limited access to basic services. In 2025, 6.4 million people required humanitarian assistance. Displacement and restricted access to healthcare have contributed to low immunization coverage among vulnerable populations. According to WUENIC in 2024, estimates show 91% coverage for the first DTP dose and 82% for the third. Challenges include underreporting, limited availability of DAT, and logistical constraints. The outbreak response is hindered by concurrent emergencies and overstretched health services.
Mauritania
From 1 January to 2 November 2025, Mauritania has reported 849 suspected cases of diphtheria and 33 deaths (CFR 4%), with 318 confirmed cases. After an initial delay, the outbreak was officially declared on 25 September 2025 and has rapidly expanded across 11 out of 53 departments (21%). An upsurge of cases has been observed since late September. The most affected age groups are children and adolescents aged 5–19 years, and women account for 60% of suspected cases. Only 10% of cases have documented vaccination history. Mauritania hosts the largest refugee camp for Malians, with over 118 000 refugees, mostly women and children. The outbreak coincides with a Rift Valley fever outbreak in some of the same regions. Response efforts are challenged by limited resource mobilization, weak active case finding, and insufficient community sensitization. Reactive vaccination campaigns have been initiated, but gaps remain in funding, logistics, and healthcare worker training. According to WUENIC in 2024, the immunization coverage is relatively high (95% for the first DTP dose and 86% for the third), but subnational disparities persist.
Niger
From 1 January to 2 November 2025, Niger has reported 1 926 suspected diphtheria cases and 122 deaths CFR (6.3%), with 765 laboratory-confirmed cases. The outbreak has affected 34 out of 72 health districts (47%) across eight regions, with most cases concentrated in Agadez, Diffa and Zinder. Compared to 2024, there have been fewer reported cases and deaths, but transmission remains active. Niger is facing a protracted humanitarian crisis driven by insecurity, climate related disruptions, economic pressures, and displacement. An estimated 2.6 million people require humanitarian assistance. According to WUENIC in 2024, the immunization coverage is relatively high (95% for the first DTP dose and 86% for the third), but recent outbreaks highlight gaps in vaccine access and delivery. A vaccination campaign in September 2025 achieved high coverage, and a second round is planned. Challenges include limited diagnostic and treatment capacity, insufficient vaccine quantities, low public awareness, and funding constraints.
Nigeria
Nigeria continues to report the highest number of diphtheria cases in the African Region. From 1 January to 2 November 2025, 12 150 suspected cases have been reported, with 8 587 confirmed and 884 deaths (CFR 7.2%). Confirmed cases have been reported from 240 Local Government Areas across 30 states. Most cases are clinically compatible, with only 3% confirmed by laboratory testing. The outbreak has disproportionately affected children and adolescents, with low vaccination coverage contributing to the spread. In Nigeria more than 2 million children are under-immunized, including those with zero-doses, highlighting the high risk of further spread. Reactive campaigns have been conducted in Imo, Kaduna and Lagos, targeting health workers and priority populations. The outbreak overlaps with areas targeted by the Big Catch-up initiative. Challenges include delayed laboratory confirmation, poor IPC practices, limited information, education and communication materials, and vaccine shortages. Discussions with Gavi are ongoing to secure additional support. According to WUENIC in 2024, the estimates show 71% coverage for the first DTP dose and 67% for the third.
South Africa
From 1 January to 26 October 2025, South Africa has reported 106 diphtheria cases, including 66 laboratory-confirmed respiratory cases, two laboratory-confirmed cutaneous cases, one probable respiratory case, and 37 asymptomatic carriers. The outbreak has affected 5 of 9 provinces (55%), highlighting the involvement of multiple provinces. Most cases and carriers are from the Western Cape, with additional clusters in Limpopo, Gauteng, KwaZulu-Natal, and Mpumalanga. CFR among probable and confirmed respiratory diphtheria cases was 18% (12/67). Most respiratory cases occurred in adults aged 18 years and older. Clusters have been documented among vulnerable populations, including individuals in correctional facilities. According to WUENIC in 2024, the immunization coverage remains below 80% in most provinces (76% for the first DTP dose and 74% for the third), and immunity gaps are widening. The outbreak response is challenged by competing priorities, limited human resources, and limited global supply of diphtheria antitoxin. Detailed case investigations and in-depth risk assessments are needed to guide targeted interventions.
Geographical distribution of diphtheria outbreaks in the WHO African Region, January 2025 until 2 November 2025
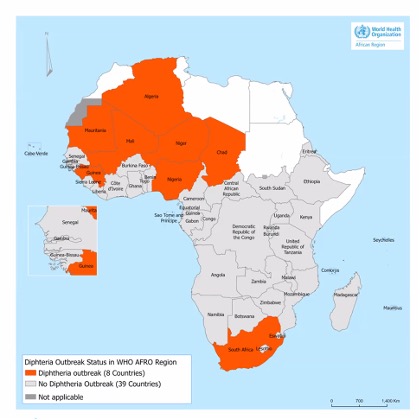
Table 1. Summary of reported ongoing diphtheria outbreaks in the WHO African region, January – 2 November 2025
 |
|---|
Table 2. Summary of vaccination coverage by diphtheria-affected country (WUENIC, 2024)
Epidemiology
Diphtheria is a severe infectious disease caused by the gram-positive bacterium Corynebacterium diphtheriae or, less commonly, toxigenic strains of other Corynebacterium species. Infection may lead to respiratory disease, cutaneous disease, or an asymptomatic carrier state. The primary mode of transmission rests on close contact with infectious material from respiratory secretions or from skin lesions. The only known reservoir for C. diphtheriae are humans. As a result, asymptomatic carriers play a critical role in infection transmission. Immunity (either via natural infection or vaccine induced) provides protective immunity against the disease but does not prevent carriage. The disease can affect all age groups; however, unvaccinated or partially vaccinated individuals, including children, are most at risk.
Respiratory diphtheria typically presents two to five days after exposure with sore throat, malaise, cervical lymphadenopathy, and low-grade fever. Oropharyngeal involvement is most common, but infection may extend to the nasopharynx, larynx, and tracheobronchial tree. Characteristic findings include adherent gray pseudomembranes on the respiratory tract mucosa that often bleed when removed. Severe cases can result in airway obstruction with neck swelling, hoarseness, stridor, or palatal paralysis. Toxin-mediated complications from toxigenic strains may include myocarditis, neurologic deficits, and kidney injury. Cutaneous diphtheria presents as chronic, nonhealing sores or shallow ulcers covered by a dirty gray membrane, though the appearance is non-specific.
In addition to supportive care, treatment is based on the appropriate administration of DAT and antibiotics (azithromycin or penicillin).
Full primary series and required booster doses. DAT administration against diphtheria has been effective in reducing the deaths and illness from diphtheria dramatically. Diphtheria is fatal in 5 to 10% of cases, with a higher mortality rate in young children. However, in settings with poor access to DAT, the CFR can be as high as 40%.
Public health response
WHO, together with its partners, continues to support national authorities in responding to ongoing diphtheria outbreaks across affected countries. Assistance focuses on both technical and operational needs.
At the country level, the scope of response operations varies according to available capacities, but core interventions remain consistent. These include enhanced surveillance through active case finding and timely reporting; adequate clinical management, including the appropriate use of antitoxin and antibiotics; risk communication and community engagement to improve public awareness and encourage care-seeking; and capacity-building efforts such as training and dissemination of evidence-based guidelines. Country-specific actions and priority needs differ, ranging from strengthening surveillance and coordination to scaling up vaccination, laboratory capacity, and medical supplies.
Despite these efforts, multiple challenges continue to hinder the effectiveness of outbreak control. Competing health priorities have contributed to long-standing immunity gaps, reflected in persistently low vaccination coverage, especially in fragile settings. Similarly, case management capacity is also limited due to scarcity of diphtheria antitoxin and late presentation of patients, resulting in high case fatality rates, especially in vulnerable, marginalized and hard-to-reach populations. In some settings, surveillance systems remain fragile, resulting in delayed detection and incomplete reporting. Limited laboratory capacity further complicates the response, with shortages of diagnostic supplies, weak specimen transport systems, and restricted technical expertise leading to delayed confirmation and underestimation of outbreak magnitude.
WHO risk assessment
Diphtheria is a major public health problem in the African region despite substantial efforts on immunization activities over the past three decades. Between 2000 and 2024, 75 789 diphtheria suspected cases were reported in the Region with the majority being reported from 2023 to 2024. In 2023-2024, Algeria, Chad, Gabon, Guinea, Mali, Mauritania, Niger, Nigeria and South Africa reported resurgence of diphtheria outbreaks with approximately 57 000 suspected cases and 2000 deaths (CFR of 3.5%) recorded. The countries most affected were Guinea, Niger and Nigeria. Most cases reported were children under fifteen years and female. Over 50% of suspected cases were non-vaccinated or with unknown vaccination status.
Since the beginning of 2025 and as of 2 November 2025, eight countries in the Region have reported a total of 20 412 suspected diphtheria cases, including 1 252 deaths (with an average case fatality ratio [CFR] of 6%). Most cases are among children and young adults, with women slightly more affected than men. Laboratory confirmation remains low due to shortages of diagnostic supplies and limited testing capacity. The global shortage of DAT, and a variable clinical capacity to provide this essential treatment, poses an additional challenge to effective case management.
Many of the affected countries are fragile, conflict-affected or have system vulnerabilities where health systems are overstretched, routine services are disrupted and access to essential services is limited. These settings are characterized by low routine immunization coverage, high population mobility, and crowded living conditions, especially among displaced populations. The resurgence of diphtheria in these countries is further compounded by disruptions caused by the COVID-19 pandemic, which led to significant declines in vaccine uptake and widened immunity gaps.
At the regional level, the public health risk is assessed as high due to the potential for further geographic expansion of outbreaks, high fatality rates, insufficient resources for outbreak control, and weak surveillance and laboratory systems. The humanitarian context in several affected countries, including Chad, Mali, Niger, and Nigeria, increases the likelihood of sustained transmission and complicates response efforts.
At the global level, the public health risk is considered low. Most countries outside the African Region have established immunization programs and adequate surveillance systems. However, the possibility of international spread through travel cannot be ruled out, particularly if susceptible individuals are exposed. Strengthened global surveillance and risk communication are therefore essential to mitigate this risk.
The confidence in the available information is assessed as moderate. While data collection and reporting have improved in some countries, gaps remain in laboratory confirmation, case classification, and timely sharing of epidemiological updates.
WHO advice
Diphtheria is a vaccine-preventable bacterial disease caused by Corynebacterium diphtheriae. It primarily affects the upper respiratory tract and can produce a toxin that leads to severe systemic complications, including myocarditis, kidney failure, and neurological damage. The disease spreads via close contact with respiratory secretions or skin lesions. Areas with low immunization coverage, overcrowding and limited access to healthcare services are at higher risk of increased transmission and may experience outbreaks
Considering the ongoing diphtheria outbreaks in the WHO African Region, WHO encourages Member States to strengthen preparedness and response capacities. This includes enhancing surveillance systems to improve case detection and reporting, expanding laboratory capacity for timely confirmation of cases, and improving clinical management and infection prevention and control. Supplementary immunization activities should be prioritized to close immunity gaps, particularly among children/adolescents and displaced populations. Community engagement and risk communication efforts must be intensified to raise awareness, promote health-seeking behavior, and ensure adherence to control measures.
WHO also recommends the establishment of contingency stockpiles of diphtheria antitoxin, antibiotics, and laboratory supplies at regional hubs in Dakar and Nairobi. These stockpiles will enable rapid deployment of essential materials to the affected countries when needed.
Regional and global advocacy efforts should be strengthened to mobilize funding and political support for outbreak response. WHO will continue to support Member States through technical assistance, resource mobilization, and coordination with partners.
WHO will continue to work across all levels of the organization to identify and implement appropriate mechanisms to support affected countries and mitigate the impact of the outbreaks.
WHO does not recommend any restriction on travel to or trade with the countries named in this report, based on the information available on the current event.
Further information
- World Health Organization. Clinical management of diphtheria: guideline. 2024 Feb 2. Available from: https://www.who.int/publications/i/item/WHO-DIPH-Clinical-2024.1
- World Health Organization. Diphtheria: fact sheet. [cited 2025 Feb 17]. Available from: https://www.who.int/news-room/fact-sheets/detail/diphtheria
- World Health Organization. Guidance on safe and supportive care in community care centres for individuals with mild mpox in camps for internally displaced persons or refugees. Available from: https://iris.who.int/server/api/core/bitstreams/32cf71ef-fd54-4cf9-ad6a-257315903018/content
- World Health Organization. Diphtheria, tetanus toxoid and pertussis (DTP) vaccination coverage. Available from: https://immunizationdata.who.int/pages/coverage/dtp.html
- World Health Organization Africa Region. Fragile, conflict-affected and vulnerable (FCV) countries. Available from: https://www.afro.who.int/node/20024
- World Health Organization. Infection prevention and control and water, sanitation, and hygiene measures for diphtheria in health-care settings: operational guide. 2023. Available from: https://www.who.int/publications/i/item/9789240088160
- World Health Organization; UNICEF. WHO/UNICEF estimates of national immunization coverage (WUENIC). Available from: https://immunizationdata.who.int/
- Bita Fouda AA, et al. Resurgence of diphtheria outbreaks in the African Region 2023–2024. Pan Afr Med J. 2025;51(1). Available from: https://www.panafrican-med-journal.com/content/series/51/1/29/full
Citable reference: World Health Organization (21 November 2025). Disease Outbreak News; Diphtheria in the African Region. Available at: https://www.who.int/emergencies/disease-outbreak-news/item/2025-DON588
