
Western Pacific Region
WPRO: Regional Appeal
- Requirements (US$): 63.1 million
Context
The Western Pacific Region (WPR) is home to approximately 1.9 billion people living in 37 diverse countries and territories. The Region is prone to Public Health Emergencies (PHE) not only from natural hazards but also from communicable disease outbreaks, including those due to vaccine preventable diseases and human avian influenza. The region also has several hard-to-reach and vulnerable populations such as those in the Pacific Islands.
Over the past two years, COVID-19 has impacted the region immensely with distinct and concerning waves associated with the Delta and Omicron variants, requiring a huge coordination of response efforts among WHO, governments and partners. Since the last wave in January 2022, the region has seen an overall declining trend in reported COVID-19 cases and deaths, though several countries experienced significant surges driven by the BA.5 subvariant at the end of June 2022. As of 20 December 2022, one country in the region, Tokelau, has not reported any confirmed cases of COVID-19.
The repeated surges of COVID-19 required many Member States to adapt their COVID-19 care pathway and enhance Infection Prevention and Control (IPC), clinical management, diagnostic capability, communication and community engagement efforts. Member States in the Region need to sustain ongoing efforts to strengthen the health delivery system and response strategies, both for COVID-19 and concurrent emergencies that affect the Region. The Region also needs to strengthen preparedness and readiness for a future pandemic or other public health emergency. Common challenges identified include the fragmentation of data systems, the incomplete utilization of health care capacity data for decision-making, an inadequate capacity and shortage of trained public health workforce including epidemiologists and laboratory technicians, the continued use of paper-based surveillance information systems and timely and effective communication.

Regional Priorities
Our priority is to support and coordinate response efforts to COVID-19 and potential future pandemics. We will build upon lessons identified during the pandemic and other public health emergencies. This will further strengthen WHO’s preparedness, readiness and response to the multiple emergencies that continuously arise in the Region.
Core priorities for the region include:
- Early detection of events to rapidly respond to emergencies:
- Strengthening monitoring of event-based surveillance sources and providing timely risk assessment as required to provide appropriate rapid response.
- Supporting Member States to further strengthen surveillance by integrating COVID-19 into the existing influenza-like illness (ILI)/ severe acute respiratory infections (SARI) surveillance system for timely detection of a surge and calibration of response measures accordingly.
- Monitoring health care capacity and supporting Member States to develop/ adapt tools and guidelines for early detection and risk assessment of an emerging respiratory virus or other public health emergency.
- Strengthening antimicrobial resistance (AMR) pathogen surveillance, antimicrobial stewardship and antimicrobial consumption monitoring so that the misuse and overuse of antibiotics are reduced to reduce the emergence of AMR pathogens.
- In response to the 2021 Asia Pacific Strategy for Emerging Diseases and Public Health Emergencies (APSED) Technical Advisory Group (TAG) meeting, continue to strengthen regional and national genomic surveillance capacity through the Emerging Molecular Pathogen Characterization Technologies (EMPaCT) Surveillance Network
- Using the EMPaCT seven-step approach, provide training modules to strengthen sub-national level public health laboratory networks and genomic surveillance (adapted to the local context) to Member States, as recommended by the 2021 EMPaCT Surveillance Network meeting.
- Strengthening laboratory capacity for facilitating access to referral laboratories and for accreditation of national food analysis laboratories
- Ensuring health care facilities can respond to demands and mitigate risks from COVID-19, other communicable diseases and PHEs:
- Establishing and sustaining COVID-19 care pathways that are integrated into primary health care systems and ensure individuals who test positive for SARS-CoV-2 are immediately linked to a clinical care pathway.
- Strengthening sustainability of IPC systems in countries, including model terms of reference for effective IPC program governance, monitoring and evaluation at health care facility level and developing more robust health care-associated infection surveillance systems.
- Strengthening water, sanitation and hygiene (WASH) in health care facilities as a core fundamental component of an integrated health care system including IPC, health care waste management and environmental cleaning.
- Strengthen the network of partners from a range of technical areas to be able to take a One Health approach that identifies and minimizes the risk of re-emergence of high-threat pathogens and the emergence of new and unknown pathogens, including coronaviruses and other zoonotic pathogens that spread between animals and people.
- Increase multisectoral coordination and collaboration at national and sub-national levels to identify gaps in key technical areas of the human-animal-environment interface, supporting the understanding of risks related to health emergencies and considering joint actions toward pandemic prevention preparedness and response.
- Support Member States to assess and improve national food safety incident and emergency response plans by strengthening their participation in the International Food Safety Authorities Network (INFOSAN) and reinforcing its interactions with IHR focal points.
- Reinforce the advocacy and implementation of public health risks mitigation measures in Traditional Food Markets at regional, national and local levels with a focus on the reduction of risks associated with food safety, zoonoses and infectious respiratory diseases.

- Develop strategic regional and national plans and conduct evaluations to measure progress
- Develop a new biregional health security action framework to protect populations of the Asia Pacific region from the impacts of public health emergencies. The framework will build on the achievements of APSED over the past sixteen years and integrate the experiences and lessons identified from preparedness and response to public health emergencies in our regions over the past two decades.
- Support Member States to plan and implement IHR Joint External Evaluations (JEEs) of their IHR core capacities. Findings from JEEs are recommended to be used to develop multiyear national action plans to ensure operational readiness for public health emergencies.
- Support countries to develop, improve and implement national action plans for health security (NAPHS) based on an all-hazards, multisectoral, whole-of-government approaches, integrating priorities and recommendations identified in JEEs.
- Support development and implementation, as well as monitoring and evaluation of AMR national action plans for Member States to accelerate actions to avert the impact of AMR in the long term.
- Strengthen the public health workforce and rapid response teams
- Continue to strengthen Field Epidemiology Training/Field Epidemiology Training Program (FET/FETP) and rapid response team (RRT) capacity to meet needs of each Member State.
- Continue to foster development, establishment and expansion of key networks and partners, including Emergency Medical Teams (EMTs) and the Global Outbreak Alert and Response Network (GOARN) to strengthen preparedness, readiness and response actions across the region.
- Further develop and maintain the capacity to support member states in preparedness, readiness and response to Public Health emergencies
- Support appropriate training, implementation and use of systems and tools including the Emergency Response Framework (ERF), use of Incident Management Systems (IMS) and structures and Emergency Operations Centers (EOC) at national and sub-national levels.
- Support readiness of member states through the development and dissemination of capacity building activities including training, simulation exercises and drills.
- Ensuring operations support and logistics for immediate response and strengthening the health system.
- Maintain the Regional Emergency Stockpile as a key resource to Member States to rapidly access critical supplies including personal protective equipment (PPE), laboratory supplies and biomedical equipment.
- Provide access to medical-grade oxygen and support the medical oxygen scale-up initiative and continue to provide technical support to Member States in need to set up domestic systems and domestic capacity for patients needing medical oxygen.
- Deploy pressure swing adsorption (PSA) oxygen-generating plants is ongoing to support priority Member States in long-term capacity-building and strengthening of the health system.
- Strengthen regional and national supply chains so that they are flexible, responsive and resilient. This will support countries to reduce costs and help ensure that essential vaccines, medicines and health products can reach the most vulnerable and hard-to-reach populations in a timely way.
- Strengthening risk communication strategies
- Provide support for Member States to develop, assess and improve national risk communication plans, including identifying and training national leaders in food safety risk communication.
- Provide timely, community-led, data-driven, collaborative communication, adapted to the local context, language and culture to help mitigate risk, reinforce capacity and develop local solutions. Particularly efforts to respond to mis- and disinformation.
- Develop and adapt COVID-19 response measures based on the latest available scientific evidence and data for the sustained management of COVID-19 as well as for use in other outbreaks or emergencies.
Facilitating information, monitoring and evaluation on COVID-19 vaccination, through the application of strategies aligned with the Regional Strategic Framework for Vaccine-Preventable Diseases and Immunization in the Western Pacific (RSF) 2021-2030. The region will continue to apply these two strategies through analysis of information and data from weekly COVID-19 vaccination and safety updates and other sources shared with WHO vaccination focal points through an internal dashboard.

A seven-member team of PNG’s National Emergency Medical Team (EMT) was deployed to Vanimo on 12 September 2021, on a 14-day mission to support West Sepik’s COVID-19 response and their surge in critical COVID-19 cases.
Focus Countries
The Western Pacific Region faces logistical challenges in delivering necessary services and materials to small island states, climate change effects that disrupt the ecosystem and affect the health and health systems of Member States and the additional challenges of competing acute emergencies such as volcanic eruptions, flooding and measles, dengue and cholera outbreaks that stretch already limited resources. Therefore, the Regional Office will continue to support all 37 countries and territories in their response efforts through tailored support based on the country context. Through the Health Emergency Appeal, WHO, in collaboration with governments and other developmental partners, are supporting 1.9 billion people for response. Response efforts will be aligned along the regional priority areas: Surveillance and Laboratory, Health Service Delivery, Strategic Frameworks and National Plans, Partnership and Coordination, Food Safety, Operation Support and Logistics, Communication and Vaccination. The total funding requirement is estimated at $USD 63.1 million.
Success stories
Reaching remote communities across the Western Pacific
Countries across the Western Pacific Region are continuing efforts to reach vulnerable, at-risk groups located in remote areas with vaccines to protect them against severe illness and death from COVID-19. Reaching every group with vaccination is crucial for protection against severe disease and death, reducing the risk of transmission and mutation of the virus, protecting the health system and supporting ongoing social and economic recovery.
In Manila, Philippines, for example, WHO helped transport people who were vulnerable to COVID-19 but had missed out on receiving a vaccine because of stigma, lack of money or residential address, difficulty accessing vaccine registration, or other barriers, to a special vaccination center. In Viet Nam, mobile vaccination teams made home visits for older adults and people with disabilities who were unable to get to health facilities. As information is just as important for people living in remote, ethnic minority communities, the mobile communication officers in Viet Nam also broadcast COVID-19 messages using loudspeakers mounted on their motorbikes and shared reliable health advice in local languages during house-to-house visits.
In order to increase vaccination rates among migrants, the Malaysian Ministry of Health had to first overcome their lack of access to information. The Government, with WHO’s support, developed tailored information materials and translated them to ensure that all communities had equal access to information about vaccines.
In the Pacific region, vaccination is challenging due to small populations dispersed over vast areas. One specific challenge was vaccinating people in Tonga’s remote Ha’apai islands, which were heavily affected by a volcanic eruption and a tsunami in December 2021. In addition to providing technical advice, WHO sent 10 000 kg of medical equipment, PPE, laboratory supplies and medicines to Tonga and worked with the Ministry of Health to establish and train the Tongan Emergency Medical Assistance Team (TEMAT), which provided medical care in the aftermath of the volcanic eruption. In addition, more than 1.2 million doses of COVID-19 vaccines were provided to Pacific Island countries via the COVAX facility. This helped achieve high vaccination rates across many Pacific Island countries and areas, including those that had not yet recorded a single COVID-19 case.
WHO’s work supporting countries across the Region to reach people with vaccines against COVID-19 is made possible by the support of donors and partners including through COVAX, which is co-led with the Coalition for Epidemic Preparedness Innovations (CEPI) and Gavi, the Vaccine Alliance, alongside the United Nations Children’s Fund (UNICEF) as a key delivery partner.

Financial requirements
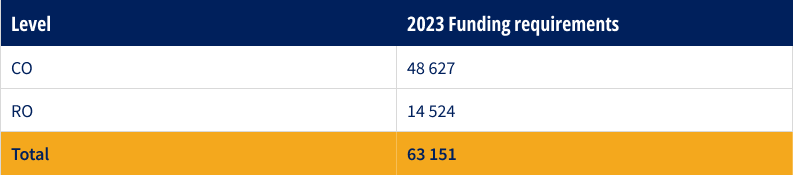
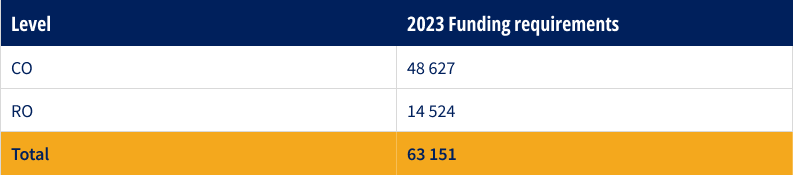
Overall regional funding requirements for ongoing emergency response operations (US$’000)
Overall regional funding requirements for COVID-19 and other emergencies (US$’000)


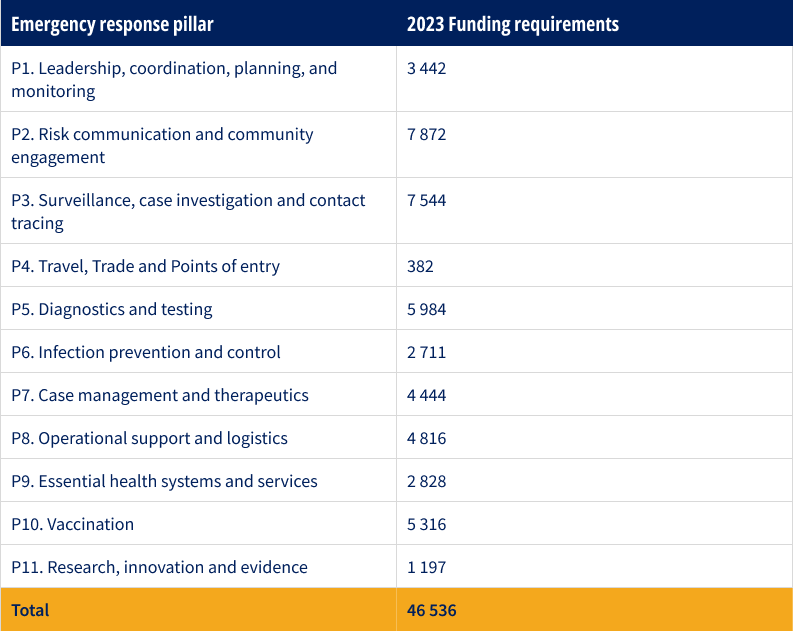
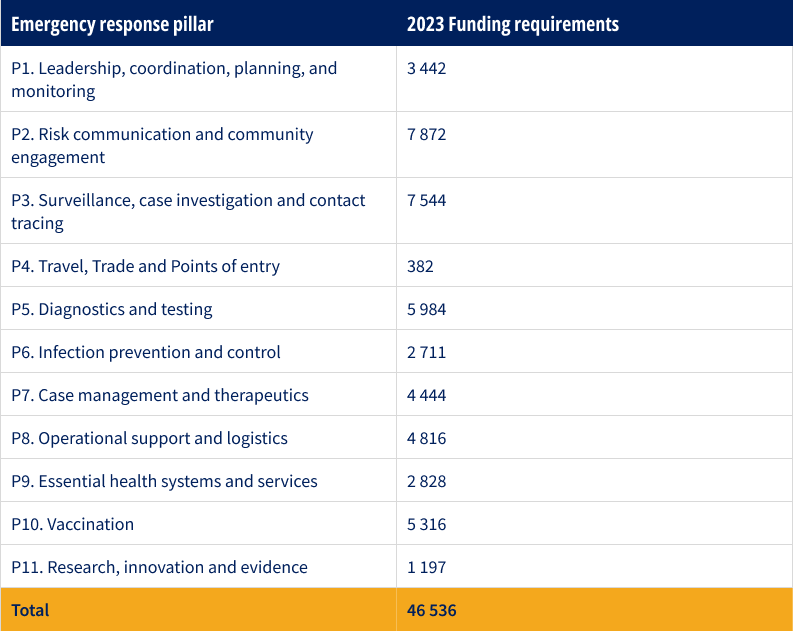
Overall funding requirements by pillar for COVID-19 (US$’000)
For more information
Dr Babatunde Olowokure | Regional Emergency Director, WHO Regional Office for the Wester Pacific | olowokureb@who.int
Ms Kristine May Nacion | Programme Area Manager (Management and Administration), WHO Regional Office for the Wester Pacific | nacionk@who.int

