
African Region
AFRO: Regional Appeal
- Requirements (US$): 604.4 million
Context
The WHO African Region (AFRO) faces the highest burden of public health emergencies globally. Conflict and climate-driven humanitarian crises, combined with new and recurrent outbreaks, are creating an increasingly complex public health emergency profile for the region. Across Member States, authorities are tackling Ebolavirus disease (EVD), cholera, meningitis, measles, Hepatitis E, mpox, yellow fever, and COVID-19, alongside situations of protracted drought and conflict.
As of November 2022, there were 132 disease outbreaks and 21 humanitarian crises being monitored, including five Grade 3 events: the Ebolavirus outbreak in Uganda, the humanitarian crisis in the Great Horn of Africa and the Sahel Region, mpox, cholera and COVID-19. Across the region, more than 133 million people are currently in need of assistance.
WHO has developed multi-level incident management systems (IMS) and strategic response plans, deployed more than 800 skilled multidisciplinary experts in all critical IMS functions to support response to major emergencies in countries, and procured essential equipment and resources.
While WHO supports countries to help curb outbreaks and meet the immediate health needs of people living through crises, through the implementation of our flagship programs we are simultaneously working to address the systemic inadequacies in the health emergency architecture in the region.
Three programs contribute towards building the capacity of Member States to adequately prepare for, detect, and respond to public health emergencies and are central to our all-hazards, longer-view, capacity-building endeavour. These are: PROSE (Promoting Resilience of Systems for Emergencies), TASS (Transforming African Surveillance Systems) and AVoHC-SURGE (African Volunteers Health Corps – Strengthening and Utilising Response Groups for Emergencies.

Maternity health unit at the national hospital in Brazzaville.
Regional Priorities
The priority for the WHO Regional Office for Africa will be to work in close collaboration with key stakeholders in the field of Emergency Preparedness and Response (EPR) to transform EPR globally.
WHO’s flagship programs PROSE (Promoting Resilience of Systems for Emergencies), TASS (Transforming African Surveillance Systems) and AVoHC-SURGE (African Volunteers Health Corps – Strengthening and Utilising Response Groups for Emergencies) are key to addressing systemic inadequacies in the health emergency preparedness and response infrastructure in the region.
Led by governments informed by technical assistance from WHO, the flagship programs will help integrate and strengthen existing national human resources for emergency response, such as Rapid Response Teams and Emergency Medical Teams. The ambition is to drive healthcare recovery in the wake of the COVID-19 pandemic beyond ‘back on track’ and instead concentrate on new high-impact interventions in the fields of preparedness and response to health emergencies, food safety and sustainable financing. WHO will also focus its efforts on urban-centered, public health capacity-building as population density and high mobility means cities are increasingly vulnerable to health emergencies.
The AVoHC-SURGE program will initially be implemented in select countries and scaled up regionally over the course of five years, aiming to create a group of 3 000 African Elite Emergency Experts equipped to respond quickly and holistically to a wide range of hazards that create health emergencies.
Regional priorities include supporting Member States to:
- Respond to emergencies through the deployment of additional experts to address human resources gaps.
- Ensure the continuity of essential health services during outbreaks and humanitarian crises, as well as the provision of quality care to crisis-affected populations.
- Strengthen early warning systems, including scaling up event-based, pathogen and genomic surveillance activities.
- Develop and use comprehensive electronic health databases that aggregate as many data sources as possible.
- Promptly share data on emergencies as required by the International Health Regulations (2005) and analyze data for decision-making.
- Strengthen and integrate the emergency workforce to ensure the availability of trained human resources at national and subnational levels.
- Strengthen response readiness and coordination to improve planning and cohesion across ministries, partner agencies and civil society organizations.
- Ensure efficient pre-positioning and deployment of emergency supplies at national and subnational levels.
- Enhance risk communication and community engagement to convey public health threats in a transparent, timely and coordinated manner through mechanisms built into National Action Plans for Health Security.
- Scale up emergency vaccination to end the acute phase of epidemics.

Focus Countries
Burkina Faso
- People in need: 4.7 million
- People targeted: 3.1 million
- Funding requirements: (US$)12.3 million
Burkina Faso continues to experience high insecurity due to political instability. More than 1.7 million people were forced to leave their homes in 2022 and are now living in precarious conditions. Since January 2022, 79 alerts relating to a security threat have already been published. The demand for health care has increased sharply as the attacks further impact and reduce the number of functional health facilities. Numerous epidemics are affecting the population, in particular measles, polio, Cholera, COVID-19 and Hepatitis E, resulting in serious health and socio-economic consequences. As of October 31, 2022, 606 health facilities had been affected by insecurity across the eight regions most affected by the current crisis, of which 32% are now completely closed. In 2023, a total of 2.8 million people will need urgent health care.
WHO is committed to ensuring equitable access to quality health services and strengthening health systems in the context of these security crises. The Organization’s response priorities include deploying mobile clinics to provide essential physical and mental health care, strengthening the transfusion capacity and availability of oxygen for the management of malnourished children, ensuring the vaccination of internally displaced people and host communities against preventable diseases, and distributing health emergency kits (cholera, COVID-19, gender-based violence, trauma, dignity kits). WHO will also prioritize building resilience through community education and awareness-raising.
Cameroon
- People in need: 4.7 million
- People targeted: 2.8 million
- Funding requirements: (US$)22.3 million
Cameroon continues to experience humanitarian and health impacts from ongoing security crises, which currently affect seven of the 10 regions in the country. As of October 2022, there were an estimated total of 481 000 Central African and Nigerian refugees in Cameroon, one million internally displaced persons (IDPs) and 519 000 returnees or former internally displaced persons who had returned to the main regions affected by armed conflict and terrorist attacks.
Since October 2021, Cameroon has been facing the longest and the most-widespread cholera outbreak since 1970. The country also faces other epidemics such as mpox, polio, yellow fever, measles and COVID-19. WHO’s support will ensure equitable access to quality health services in the context of these security crises. The Organization’s response priorities include deploying mobile clinics to provide essential health care, including reproductive health services. Support will be offered for dignified and safe deliveries for vulnerable women, and gender-based violence cases will be referred to the protection sector. Focus will be placed on establishing an early warning and rapid response to epidemics mechanism for regions in crisis, as well as strengthening the management of physical and psychological trauma for people affected by crises. WHO will also prioritize building resilience through community education, awareness-raising and empowerment.
Central African Republic
- People in need: 3.4 million
- People targeted: 2.4 million
- Funding requirements: (US$)8 million
For more than nine years, the Central African Republic (CAR) has been facing a socio-political and military crisis, generating a chronic humanitarian crisis with acute episodes linked to armed conflicts and floods. This has led to population displacement, reduced health system capacity and epidemic outbreaks. As of October 2022, there were an estimated 505 000 internally displaced persons (IDPs) in CAR, of whom 141 000 live in refugee camps. The country is threatened by several epidemics, including measles, pertussis, yellow fever, mpox, canine rabies, vaccine-derived polio and COVID-19. In addition, the country continues to face other diseases, which are the main causes of morbidity and mortality, including malaria, respiratory diseases and diarrheal diseases. Beyond the country's poor epidemiological profile, attacks on the health system continue, with 19 such attacks in 2022. An estimated 2.9 million people will need emergency health assistance in 2023.
WHO’s interventions will support humanitarian partners and the Ministry of Health in priority areas for the provision of emergency health services. WHO’s strategy will focus on capacity building to prepare for and prevent epidemics and other health emergencies, supporting the country in building capacity for timely detection, rapid reporting, and confirmation of all outbreaks and other health emergencies, and ensuring effective coordination to improve access to essential health services for the most vulnerable populations.
Chad
- People in need: 6.9 million
- People targeted: 4.5 million
- Funding requirements: (US$)10.8 million
The humanitarian crisis in Chad is impacted by multiple factors, including ongoing armed conflicts, economic fragility, a precarious health context, the impacts of climate change, flooding, acute food insecurity and associated infectious disease epidemics. More than 2.1 million people are in food and nutrition insecurity in Chad.
The decline in agro-pastoral productivity is affecting the nutritional status of the population. From September 2022, heavy rains have battered the country's south, causing the Chari and Logone rivers, which meet in the capital city of N'Djamena, to overflow their banks, forcing 149 936 people to flee their homes and take refuge in public spaces.
Chad is also affected by circulating vaccine-derived poliovirus type 2 (cVDPV2).
WHO’s response strategy will focus on scaling up its response in collaboration with existing health facilities and Health Cluster partners, enabling mobile clinics in areas which are difficult to access or without functional health facilities, improving early warning systems and implementing community-based surveillance for early detection of potential epidemic diseases.
Democratic Republic of the Congo (DRC)
- People in need: 26.4 million
- People targeted: 10.0 million
- Funding requirements: (US$)41.1 million
The health situation in the DRC is marked by the emergence and re-emergence of several communicable diseases with epidemic potential. During the last decade, the occurrence of several epidemic outbreaks, including cholera, Ebolavirus disease (EVD), polio, measles, mpox and COVID-19, in a context of humanitarian crisis related to the volcanic eruption of Nyiragongo and fighting between the regular army and rebel groups, have led to massive displacement of the population. A total of 5.7 million civilians have been displaced and are now living in collective centers (churches, schools, stadiums) and refugee camps.
WHO’s response strategy will focus on the humanitarian crisis, cholera, and COVID-19. In addition, WHO will also continue to support readiness and response for Ebolavirus disease, polio, measles and mpox. WHO will support the continued provision of essential health services, including responses to gender-based violence, mental health and psychosocial challenges. The Organization will focus on strengthening the health system while rapidly responding to acute health emergencies through the development of local capabilities.

Nurse Fatuma Ahmed vaccinates Aisha's 45-day-old baby Hamfery at Aysaita General Hospital on 20 October 2022.
Ethiopia
- People in need: 28.6 million
- People targeted: 26.6 million
- Funding requirements: (US$)128 million
Ethiopia's health system is affected by the ongoing conflict in Tigray and a drought affecting the south and southern regions. The combined effect of these emergencies has led to a gradual disruption of the health delivery system, which is hampering the health and well-being of millions of civilians and causing internal displacement. This has resulted in negative health consequences such as heightened risk of disease transmission and the breakdown of health facilities and social services, putting millions at risk of epidemic prone diseases such as measles, cholera, meningitis, malaria, polio and ongoing COVID-19 pandemic.
To address these emergencies, WHO will continue to collaborate with the Federal Ministry of Health, the Ethiopian Public Health Emergencies Institute (EPHI), the Region Health Bureaus (RHBs), and other health partners. The key aim is to build on current health sector development initiatives, increase capacity, and incorporate risk management and resilience-building strategies to advance long-lasting solutions, which will help improve readiness for any further deterioration of the humanitarian situation. To ensure continuity of delivery of essential health services, WHO will provide material and operational support to priority health facilities. WHO will support broader implementation of public health measures to prevent and manage disease outbreaks, with a focus on malaria, cholera, measles, yellow fever, meningitis, and COVID-19. The Organization will also integrate with the essential health service delivery public health measures for disease control, including epidemiological surveillance and early warning.
Madagascar
- People in need: 1.6 million
- People targeted: 1.15 million
- Funding requirements: (US$)7.5 million
Madagascar is currently facing a chronic crisis caused by major hydro-meteorological events. A drought in the south and the recurrence of cyclones in the south-east have affected more than one million people, and 825 000 people are urgently in need of health care. The country is at high risk of outbreaks of malaria, polio and pneumonic plague.
WHO’s support will focus on disaster-prone regions at risk of cyclones, floods, droughts and epidemic diseases. WHO is committed to strengthening preparedness and response to the health consequences of drought and cyclones. The Organization’s response will reinforce strategic and operational coordination by supporting the establishment of the Public Health Emergency Operating Center (PHEOC) at regional level for rapid decision-making and action. In addition, WHO will work on reinforcing disease surveillance, increasing access to health services and improving risk communication and community engagement intervention.
Mali
- People in need: 9.0 million
- People targeted: 6.2 million
- Funding requirements: (US$)15.5 million
The humanitarian situation in Mali deteriorated significantly over the first half of 2022 due to the intensification of internal conflict and intercommunity clashes. The level of need is at its highest since the conflict crisis began in 2012. Currently, 7.5 million people, or one in three Malians, are in need of humanitarian assistance, up from 3.8 million in 2017. The number of internally displaced persons (IDPs) is increasing and more than 350 000 people have had to flee their homes. In addition, 1.8 million people are in need of food aid - a 50% increase from last year. As of November 2022, a total of 32 755 confirmed COVID-19 cases have been reported in the country, including 742 deaths. The case fatality rate is among the highest in West Africa (2%). Vaccination coverage against COVID-19 during this period was just 9.76%.
WHO’s priorities include building capacity of health care workers through training and technical supervision and reinforcing access to quality health care, including monitoring the Minimum Package of Activities and Complementary Package of Activities. Mobile clinics will be strengthened, in addition to information and referral systems, and greater support offered to conducting vaccination sessions for children targeted under the Expanded Vaccination Programme. WHO will also strengthen preparedness and response for disease outbreaks, including COVID-19, measles and other diseases. The Organization will also work to ensure that populations, especially those impacted by gender-based violence, have access to psychosocial support services.
Mozambique
- People in need: 2.0 million
- People targeted: 1.6 million
- Funding requirements: (US$)4.7 million
Mozambique is experiencing an intense humanitarian crisis due to the long-lasting armed conflict affecting the province of Cabo Delgado, resulting in over 735 000 people fleeing their homes since 2017. In addition, the country also faces the challenge of hydro-meteorological shocks, such as floods and drought. In 2023, an estimated 1.5 million people will need emergency lifesaving and life-sustaining health services across the three northern provinces affected by the conflict (Cabo Delgado, Nampula and Niassa), the provinces affected by floods (Zambezia and Sofala) and those affected by drought (Gaza and Inhambane). As a result of these crises, poor living conditions and accommodation increase the country’s vulnerability to disease outbreaks of cholera and measles among displaced people and host communities. Population displacement also increases exposure to sexual and gender-based violence for vulnerable women and children.
Mozambique is co-affected by wild poliovirus type 1 (WPV1) and circulating vaccine-derived poliovirus type 1 and 2 (cVDPV1, cVDPV2).
WHO will focus its support on providing equitable access to quality health services in the context of these crises. High impact interventions will be conducted, such as scaling up laboratory and field-testing capacity for cholera, increasing vaccination and providing sexual, reproductive health care and antenatal care.
Niger
- People in need: 4.2 million
- People targeted: 2.3 million
- Funding requirements: (US$)12.9 million
Niger is currently experiencing complex and protracted emergencies. The security situation in the country remains precarious and volatile in the border areas between Burkina Faso, Mali, and Nigeria, marked by an upsurge of attacks by non-state armed groups. The country also experiences cyclical natural disasters due to its geographic environment. In 2022, the country experienced four health crises related to epidemics (meningitis, measles, polio and cholera) in addition to the disaster caused by floods, drought, food crisis, COVID-19 and the risk of emerging and re-emerging diseases.
WHO aims to employ several strategies including supporting existing health structures to ensure equitable access to health care, deploying mobile clinics and temporary structures in refugee camps, setting up early warning systems in fragile and hard-to-reach areas and strengthening the surveillance of diseases with epidemiological potential.
Nigeria
- People in need: 8.3 million
- People targeted: 5.4 million
- Funding requirements: (US$)59 million
Tens of thousands of people have been killed and millions internally displaced since Boko Haram launched its campaign in 2009, creating one of the world's worst humanitarian crises and causing a near-total breakdown in education and health services.
Throughout the northeast region, the violence has destroyed schools, hospitals and other social facilities, leaving affected communities, particularly women and children, in urgent need of assistance. Overall, around 8.4 million people, primarily women and children, in Borno, Adamawa and Yobe states are in need of humanitarian assistance and 5.5 million people need urgent health care. The country also faces disease outbreaks among displaced populations, including cholera, Lassa fever, mpox, circulating vaccine-derived poliovirus type 2 and yellow fever.
WHO’s response to the crisis in the northeast aims to support the continued provision of essential health services including gender-based violence, mental health and psychosocial support, and strengthening the health system while rapidly responding to acute health emergencies through local capacities. This will complement the overall humanitarian response addressing health needs detailed in the Humanitarian Response Plan - 2022 and the yearly rolling WHO response plan to the northeast including coordination of the health sector.
South Sudan
- People in need: 9.4 million
- People targeted: 6.8 million
- Funding requirements: (US$)52.1 million
In South Sudan, humanitarian needs have been growing for the fourth consecutive year since 2019, mainly due to political conflict and localized violence in Upper Nile, Warrap, Unity, Jonglei, and Central Equatoria states, as well as severe flooding which has impacted 37 counties and acute food insecurity (IPC4+) affecting over 20 counties. An estimated 8.9 million people are currently in need of humanitarian and protection assistance, of which 6.1 million require emergency health services.
The Humanitarian Response Plan 2023 will target around 3.4 million people (56% of the total population) in need of emergency health services. In addition to ongoing health needs, an estimated 6.6 million people are currently at risk of food insecurity in South Sudan – a number which is projected to rise during the lean season (April-July 2023) to 7.8 million. During the same period, 1.4 million people, including 345 893 children under the age of five, are projected to be severely malnourished and will likely suffer from acute malnutrition by June 2023. In addition to the acute food insecurity and flooding situation, South Sudan is experiencing an explosive measles outbreak that has now spread to 15 counties in eight states as well as a cholera and hepatitis E virus outbreak. The country is also now in preparedness mode for a possible Ebolavirus disease outbreak following an outbreak in Uganda.
WHO’s response strategy will focus on strengthening national and sub-national preparedness and response capabilities against public health events, deploying technical experts to provide technical support and coordinate response, and strengthening the coordination between humanitarian and development actors.
Uganda
- Funding Requirement: (US$) 30.6 million
Uganda is epidemiologically vulnerable to public health emergencies arising from its geographical location in the meningitis and yellow fever belts, the ‘filo virus triangle,’ and proximity to the biodiversity rich ‘hot spot’ of the Congo basin.
The country registers the second largest number of public health emergencies in the Africa region annually and is currently hosting over 1.53 million refugees, making it the largest refugee hosting country in Africa. Malaria remains Uganda’s leading cause of death, particularly among children under five years old. The country is currently responding to three Grade 3 emergencies: Ebolavirus disease, greater Horn of Africa Drought, and COVID 19. In 2022, several disease outbreaks occurred, including malaria, Rift Valley fever (RVF), and Crimean-Congo hemorrhagic fever (CCHF) among others. Uganda is affected by circulating vaccine-derived poliovirus type 2 (cVDPV2). Uganda’s food insecurity levels remain classified as ‘serious’ according to the 2019 Global Hunger Index. Malnutrition is widespread across the country and 1.2 million people are facing severe risk of public health consequences.
WHO’s work in the country will focus on supporting epidemiological field investigations and community-based risk assessments, developing a food safety surveillance system, supporting response to floods, droughts and mudslides, and assisting implementation of the refugee response plan. The Organization will also support subnational level laboratory capacity, the procurement of essential diagnostic reagents and transport media for common pathogens, and will support rapid deployment of an adequate medical and technical workforce.

A billboard promoting Ebola awareness in Kampala, Uganda, on 7 November 2022.
Success Stories
Uganda - Contact Tracers and Village Health Teams Take on SUDV in Uganda
Contact tracers are crucial to ending the spread of SUDV which causes Ebola. Since an outbreak was declared in September 2022 in Uganda, around 300 contract tracers – volunteers trained in disease surveillance and recruited to help build trust and overcome fear among communities - have been deployed to assess if contacts are displaying Ebola disease symptoms. Each tracer works with up to 10 village health workers from the local communities.
Health assistant Nyangoma Kirrungi is a contact tracer in Madudu sub-county. On average, she follows up on 40 contacts a day. "I work closely with the investigation unit,” she explains. “Once they record a confirmed case of Ebola, my team and I go to the field to follow up with the patient's contacts to ensure that they are symptom-free and then we remain on alert to identify and report symptoms should they develop."
Communities can report suspected cases using two hotlines. Once a case is confirmed, a case investigation team establishes a list of contacts who are then located and screened. Village health teams take over the monitoring of any symptoms for 21 days ‒ the Ebola incubation period – and provide invaluable assistance in raising awareness within their communities. “When the community cooperates in the response and contacts are identified, it becomes easier to contain the disease," says Dr Bernard Logouomo, the Ministry of Health Surveillance Team Lead in Mubende District, another Ebola-hit area.
Since the start of the epidemic, the Ugandan Ministry of Health has trained over 1 200 village health team members with support from WHO. By mid-October, nearly 94% of 552 contacts were seen and monitored daily for 21 days.
Contact tracers and village health teams, however, face numerous daily challenges, including a lack of personal protective equipment, reliable transport and difficulties in monitoring contacts who may not be at home when visited. Contact tracers are also often faced with community members’ fear of being stigmatized or isolated in a health facility, which may put their livelihoods at risk.
With support from the United States Agency for International Development and the Norwegian government, WHO has provided four Ebola kits to Mubende Regional Hospital and redeployed 108 technical staff to assist with case management, risk communication, community engagement and laboratory testing.

Members of the Contact Tracing and Risk Communication teams discussing the signs and symptoms of Ebola with the community in Madudu - Mubende District of Uganda.
Niger – Ensuring quality health care insecure areas affected by non-state armed groups activism.
Niger's precarious and volatile security situation has left tens of thousands of people displaced. As a result, access to basic health care for these communities, alongside those in hard-to-reach areas remains challenging. To support the health authorities in ensuring quality health care is available in insecure areas, WHO Niger is collaborating with the local NGO “Action for Well-Being" (Action Pour le Bien Être).
As a local organization, Action Pour le Bien Être have key knowledge of the field and the acceptance of local populations. Together with WHO, the group has established mobile clinics which operate in six health districts within Tahoua and Tillabéry.
Every month, two mobile clinics provide curative care, vaccination and reproductive health services (prenatal consultations, postnatal consultations, delivery, care for newborns). In total, the initiative has reached more than 100 000 people, including 70 000 internally displaced persons and 30 000 indigenous people. The program has mobilized more than 300 community relays trained to support health workers in raising awareness and monitoring diseases with epidemic potential. In addition to these activities, six health centers involved in the mobile clinics initiative have been rehabilitated.
The program has been developed in line with the following framework: Emergency Health Assistance to Internally Displaced Populations, Refugees and Host Populations and Resilience of the Health Systems in the Context of COVID-19.

Preparation of a cholera treatment center
Financial requirements
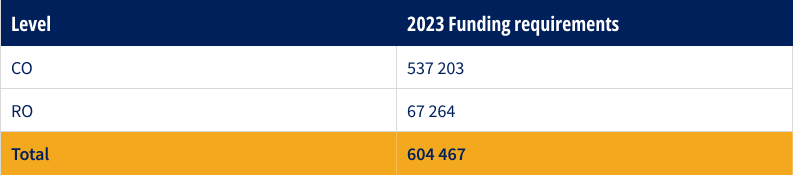
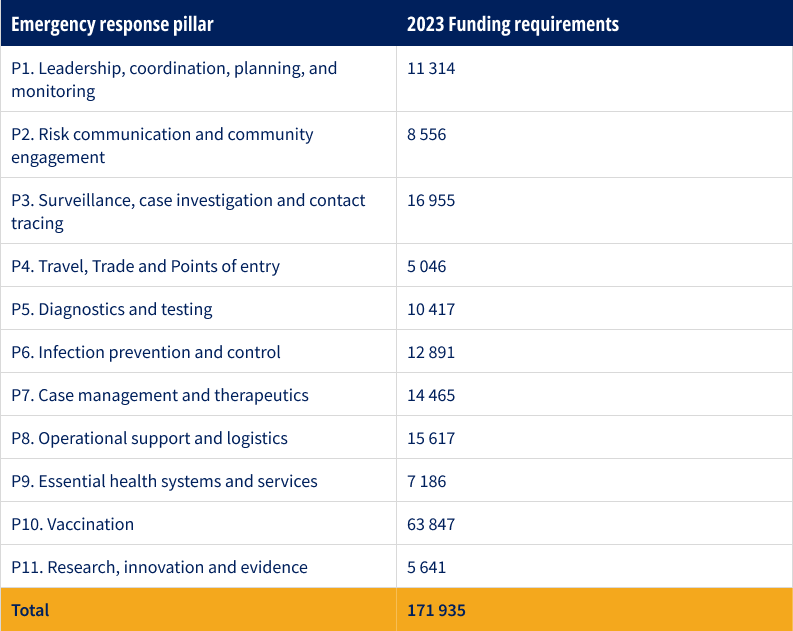
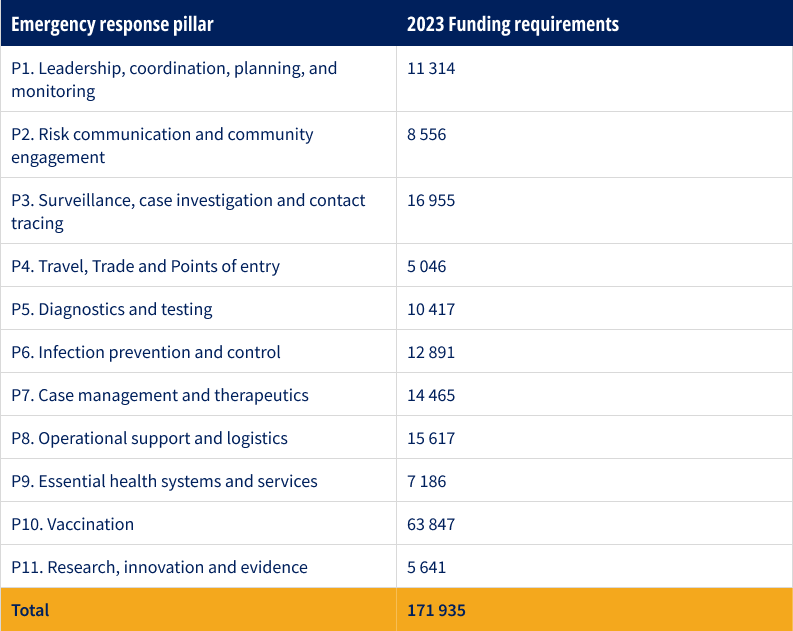
Overall regional funding requirements for ongoing emergency response operations (US$’000)
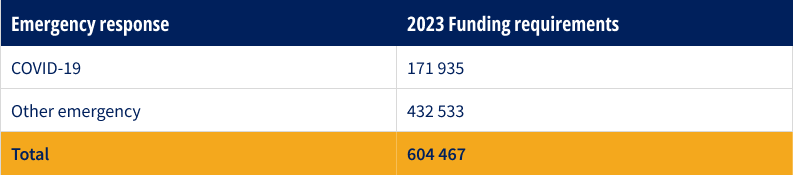
Overall regional funding requirements for COVID-19 and other emergencies (US$’000)
Overall funding requirements by pillar for COVID-19 (US$’000)
For more information
Abdou Salam Gueye | Regional Emergency Director | gueyea@who.int
Berenice Emeline Akinotcho | Resource Mobilization Officer | akinotchob@who.int
Etienne Magloire Minkoulou | Planning, Monitoring and Evaluation Officer | minkouloue@who.int

