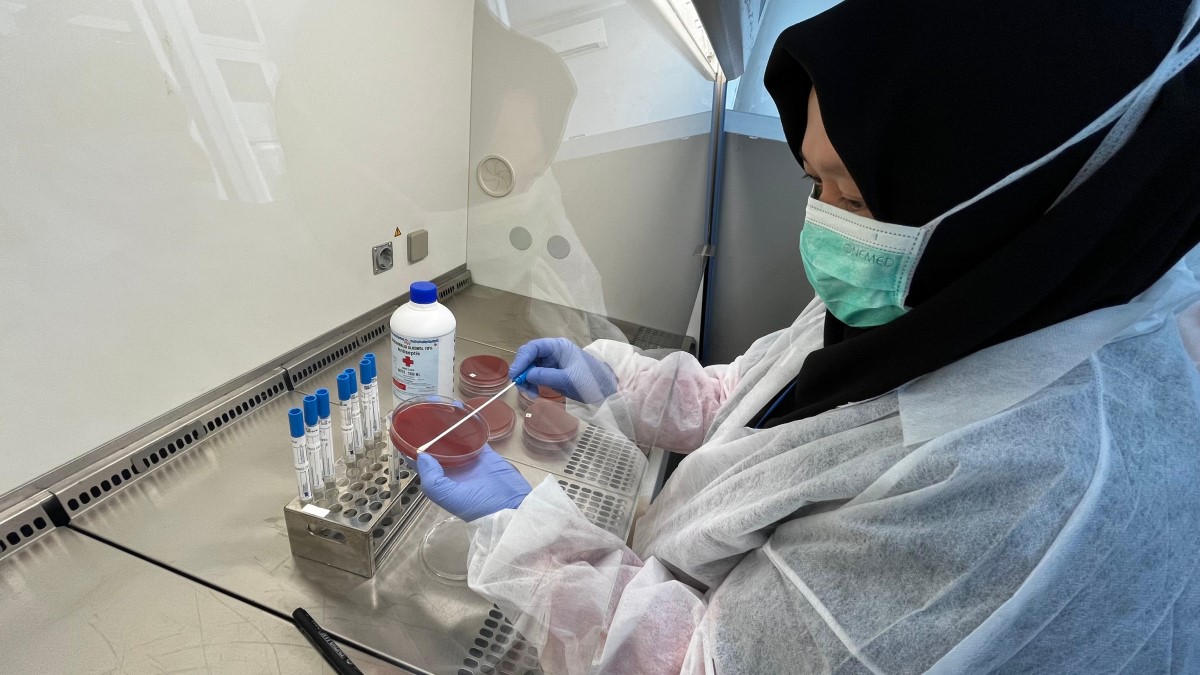
After observing the instructors grow diphtheria bacteria in blood agar dishes, training participants also attempted this process. Cystine Tellurite Blood Agar (CTBA) is a selective media used to isolate and cultivate diphtheria bacteria (Corynebacterium species). If they grow, suspect diphtheria bacteria would be seen as greyish black colonies. This method is the primary and gold standard diagnostic test for diphtheria infection. Credits: WHO/Bunga Manggiasih
From 23–29 June 2024 laboratory technicians from across Indonesia participated in hands-on training on how to carry out microscopic, bacterial and toxicity testing for diphtheria, a disease that can kill 30% of unvaccinated cases without proper treatment, with young children especially at risk.
The week-long training was conducted by the National Health Biology Laboratory, Jakarta and involved technicians from a range of at-risk and affected areas, including Ambon, Banda Aceh, Banjarbaru and Papua. It was supported by the World Health Organization (WHO) and Australian Government and will complement country-wide efforts to strengthen diphtheria case management and ensure that every child receives three primary doses of diphtheria-containing vaccine during infancy, as well as booster doses at 18 months of age and through school vaccination.
Globally, outbreaks of diphtheria have occurred with increased frequency and severity since the onset of the COVID-19 pandemic, due to disruptions of routine immunization services and surveillance activities. Between 2019 and 2021, there was an almost 40% increase in the number of unvaccinated “zero-dose” children globally, with significant variation between and within countries.
In Indonesia, gaps in routine immunization coverage resulted in 103 reported outbreaks of diphtheria in 2023, covering 68 districts and cities in 19 provinces. A total of 69 deaths were reported countrywide. Cases of diphtheria were detected and reported by eight public health laboratories at the provincial and national levels. The two national level laboratories were the National Health Biology Laboratory in Jakarta and the Regional Public Health Laboratory in Surabaya.
“Early detection of diphtheria cases and contact tracing are crucial for more effective and accurate treatment and control of diphtheria,” said dr. Endah Kusumowardani, Head of the Surveillance Laboratory Working Group, Ministry of Health, Government of Indonesia. “If diphtheria is suspected, testing should be performed promptly, and treatment started as soon as possible. This is why this training is so important, especially for communities in underserved, remote and hard-to-reach areas.”
Symptoms of diphtheria usually begin 2–5 days after exposure to the bacteria. They include a sore throat, fever, swollen neck glands and weakness. Cases of diphtheria are usually treated with diphtheria antitoxin as well as antibiotics, as detailed in WHO treatment guidelines. In both 2023 and 2024, the guidelines have been shared with health workers from across the country, through a series of webinars and workshops.
At the 23–29 June laboratory training, participants engaged in practical sessions on managing diphtheria specimens, biosafety and biosecurity, microscopic examination of specimens, and examination of specimens with culture, PCR and Elek Test methods. The training was aligned with the WHO South-East Asia Region Surveillance Guide for Diphtheria, published in September 2023, and will inform Indonesia’s immunization programming and priorities moving forward.
“Australia is pleased to partner with Indonesia and WHO to bolster laboratory and surveillance capacity to safeguard communities and mitigate health risks,” said Madeleine Scott, First Secretary Health, Australian Embassy Jakarta. “This underscores our commitment to enhancing our shared health security and resilience.”
In alignment with the joint WHO Indonesia Country Cooperation Strategy 2024–2027, WHO will continue to provide the Ministry of Health actionable support across all areas of diphtheria prevention, detection and treatment, helping to achieve the national control target, and ensuring that together, we “build forward better”.
This activity was supported by the Australian government through the Department of Foreign Affairs and Trade.
Written by Joshua Harmani, National Professional Officer (VPD Surveillance), WHO Indonesia
