The case studies in this chapter provide examples how countries planned and implemented health sector strengthening strategies and intersectoral action, and their efforts in ensuring meaningful adolescent and youth engagement in these processes.
Comprehensive Sexuality Education Programme in Zambia
In 2016, in partnership with UNESCO, the government of Zambia launched a national comprehensive sexuality education (CSE) programme addressing all young people, including those with disabilities and those living with HIV. The goal of the programme was to increase access to age-appropriate CSE for young people ages 10–24 years. Ultimately, the purpose of the programme was to improve the health of adolescents and young people by providing them with better appropriate and timely SRH education. The International Technical Guidance on Sexuality Education, developed by UNESCO and its partners, guided implementation of the programme.
The government of Zambia implemented several strategies, including integrating CSE into school curricula in all government schools from grades 5 through 12, training teachers and providing them with culturally appropriate and gender-sensitive teaching materials. The delivery and sustainability of the programme was ensured by collaboration across key sectors, including relevant government ministries, local government, UN agencies, NGOs and other partners. Ownership of the programme at the local level was built by training and tasking Provincial Standards Officers to monitor the delivery and quality of CSE at the school level.
A careful and systematic approach to implementing CSE that is evidence-based, age-appropriate and sustainable has so far resulted in positive results for schools implementing the programme. In 2015 the programme reached an important milestone – implementation of CSE in all targeted government schools across the country. An evaluation of the programme using the Sexuality Education and Review Tool found positive results, with high scores for many key metrics, including objectives, coverage, programme model, stakeholder analysis and programme content.
By 2016 nearly 77% of the programme coverage target had been met, reaching over 1.35 million learners through 38 521 teachers trained in-service by 243 master trainers.
Source: Promoting gender equality in sexual, reproductive, maternal, newborn, child and adolescent health. New York: UN Women; 2019 (https://www.unwomen.org/sites/default/files/Headquarters/Attachments/Sections/Library/Publications/2019/Promoting-gender-equality-in-SRMNCAH-Programming-guide-en.pdf).
Management of the Health in Schools programme at the local level in the Philippines – making every school a health-promoting school

About one third of the population of the Philippines is of school age, and health in schools is considered an important component of the agenda of the country’s Department of Health. Although the country does not have a direct school health policy based on WHO’s definition for HPS, it has an SHN programme that includes several interventions similar to those of WHO’s HPS approach. In July 2018 the Department of Education launched the Health in Schools programme. Its goal is to provide education on healthy lifestyle behaviour and to offer basic primary health, nutrition and dental care for school staff and students and also to ensure a link between providers of child and adolescent health services and local governments.
While the programme is led and implemented by the Department of Education, coordination of the programme depends mostly on local governments. Local governments are responsible for the management and allocation of funds to schools for the implementation of the various programmes. They receive and allocate funds from the central government as well as provide additional funding to support school improvement and other needed interventions not funded by the central budget. Local authorities such as school officials and superintendents support initiatives in SHN programmes and projects, for instance. They also provide other administrative support needed for school-based management of the Health in Schools programme.
School management also contributes to the development of school-level polices and the management of the school environment. Although barriers still exist to school health programmes, the Health in Schools strategy, by including local authorities as key stakeholders, has contributed to the success of some health programmes in schools, such as water, sanitation and hygiene (WASH).
Source: Making every school a health-promoting school: country case studies. Geneva: World Health Organization; 2021 (https://apps.who.int/iris/bitstream/handle/10665/341909/9789240025431-eng.pdf).
Formative nutrition research with adolescents in Cambodia

Who better to involve in research for adolescents than adolescents themselves? Not only will their unique perspectives and viewpoints inform the findings, but also their involvement in conducting the research can help assure its relevance and insight. This realization has prompted many stakeholders to actively engage adolescents in participatory research methodologies to inform programming.
In Cambodia, where adolescents make up about one fourth of the population, the WFP undertook research to contribute to the global evidence base on adolescents and to guide future nutrition programmes. The research, which took place in 2016 and 2017, followed a participatory research methodology that included adolescents and their communities. The objectives of the study were to assess adolescents’ nutritional needs and priorities, to understand how they prefer to engage with nutrition programmes, to ascertain the current programmatic and policy environment and to make recommendations for context-appropriate, user-centred nutrition interventions for adolescents. Data were collected from 280 participant in three provinces. Data collection used qualitative methodologies that engaged adolescents, including focus group discussions, key informant interviews, workshops and technology surveys.
The research elicited perspectives directly from adolescents on how they view and define their experience as adolescents, their food and nutritional needs, factors affecting their nutrition and how they would like to be engaged by programmes. The active participation of adolescents led to key recommendations for policy and programmatic considerations. Recommendations included investment to increase access to healthy and nutritious foods, to provide healthier food options, to keep adolescents in schools and to improve maternal health awareness as well as recommendations on food preparation and consumption and on improved land and agricultural practices. An important consideration emerging from the research findings was the importance of attention to gender roles within communities and their influence on future programmes and interventions.
Source: Formative research to inform adolescent programming in Cambodia: engagement for health, nutrition, and sustainable development. Rome: World Food Programme; 2018 (https://docs.wfp.org/api/documents/WFP-0000064044/download/?_ga=2.155210803.907460398.1664883718-1710763202.1664883718).
Youth group in Malawi equips and empowers young people

HeR Liberty, a youth-led agency established in 2017 in Malawi, has been working on adolescent-focused approaches to improve the health and well-being of adolescents. In partnership with key stakeholders, including the Global Financing Facility, the organization engages meaningfully with youth from local communities to co-create approaches. Young people are given the freedom to develop a plan to improve their health and well-being based on their needs and resources. The organization trains youth leaders and gives them toolkits so that they can complete their own financial and narrative reports for projects that they undertake. Also, youth leaders are trained how to engage local leaders and government bodies on issues related to adolescents’ health and well-being. The approach of HeR Liberty is to empower and support young people through advocacy so that they are better informed about key issues affecting their health and well-being, such as sexual health and reproductive rights.
The organization has successfully used music and short videos to develop advocacy toolkits and roadmaps in partnership with youth networks, UN agencies and other organizations. Using a clear communication and media strategy, the organization employs social, online and conventional media (radio and television) to share messages about sexual and reproductive health and rights (SRHR). By 2019 their advocacy song Inu ndi ife had played on eight radio stations and six TV channels. In addition, downloads for the song via the online platform www.malawi-music.com had surpassed 16 000 by December 2022. In one campaign, because the organization worked with youths to co-develop approaches and plans specific to their context, the organization reached 4000 youths in 30 days through eight youth leaders and over 80 youth clubs. HeR Liberty reports that, by December 2022, the organization had reached 8000 young people in 12 districts and worked with 100 youth leaders and peer educators and with 80 clubs (https://www.herlibertymalawi.com/). The organization has also organized intergenerational dialogues with over 20 community and traditional leaders in four local districts in Malawi.
Source: Rolling out the advocating for change for adolescents toolkit in five countries: highlights, challenges and lessons learned: youth advocacy brief. Geneva: World Health Organization; 2020 (https://apps.who.int/iris/handle/10665/362195).
Global Fund invests in adolescent health programmes in the United Republic of Tanzania

The Global Fund is a key funding partner investing in health and well-being initiatives specific to adolescents and young people. Globally, they have funded several initiatives on important public health issues affecting young people, including HIV/AIDS. In the United Republic of Tanzania, the Global Fund invested about US$ 1.66 billion in HIV programmes between 2002 and 2022. Recognizing that adolescent girls and young women are disproportionally affected by the disease in the country and across sub-Saharan Africa, the Global Fund, in collaboration with the Ministry of Health and local and international partners, has made several investments in programmes to reduce the vulnerability of adolescents to HIV and protect them from infection. These programmes provide girls and young women at risk of HIV with a comprehensive package of HIV preventive services tailored to their needs, including more access to HIV prevention options and knowledge of HIV prevention and other SRH issues and of how they can empower themselves and their peers.
These investments and other actions have shown very positive impacts over the last decade. The United Republic of Tanzania has made tremendous progress in the fight against HIV. Between 2010 and 2021, AIDS-related deaths and HIV incidence have been reduced by 60% and 62%, respectively. In addition, within that same period, the country has increased the numbers of people who know their status, the proportion of those living with HIV who are receiving ART and the proportion of those on ART who have suppressed viral load. The country also has increased the coverage of services for prevention of mother-to-child transmission.
Source: The Global Fund results report 2022 - world. Geneva: The Global Fund; 2022 (https://www.theglobalfund.org/media/12265/corporate_2022resultsreport_report_en.pdf).
Building teacher capacity supports student inclusion in Scotland

In 2021 Scotland embarked on work to increase teacher capacity so that schools across the country could be more inclusive of LGBTI students. The LGBTI-inclusive education policy complements other policies such as the national anti-bullying and Respect for All initiatives. The focus of the LGBTI-inclusive education policy was in line with a national policy that aims to provide both students and teachers with the requisite training and resources so that they are adequately informed about LGBTI issues at both primary and secondary school levels. Teachers and staff in primary and secondary schools across Scotland received toolkits and other resources to increase their competencies on LGBTI issues. The toolkits and resources also explained how to implement a curriculum that includes considerations specific to the LGBTI community. In addition to these resources, teachers and staff were offered in-person and virtual training sessions and a certificate of completion. According to preliminary data, almost all teachers who participated in the trainings reported increased knowledge on implementation of the LGBTI-inclusive strategy in primary and secondary schools. In addition, some teachers are also reporting increased confidence in their ability to manage LGBTI issues.
Source: McBrien J, Rutigliano A, Sticca A. The inclusion of LGBTQI+ students across education systems: an overview. Paris: Organization for Economic Cooperation and Development; 2022 (https://www.oecd-ilibrary.org/education/the-inclusion-of-lgbtqi-students-across-education-systems_91775206-en%3Bjsessionid=Xqg34ZCBv2ts1u3T_j8SBUpOnOPKLJxTA_CALrE_.ip-10-240-5-61).
Upholding the rights to education, health and basic nutrition during COVID-19 in South Africa
In the midst of the COVID-19 pandemic, schools in South Africa closed, limiting the delivery of the National School Nutrition Programme (NSNP), which provides a daily meal to all pupils in South Africa who are eligible based on economic need. The government announced that schools would reopen on 8 June 2020 and the NSNP would be restored, but, when the time came to reopen schools to some pupils, the NSNP meals were not delivered as promised.
The NSNP was introduced expressly to address both the right to basic education under Section 29 (a) of the South African Constitution and the right of children to basic nutrition under Section 28 (c). Consequently, the authorities had a constitutional duty to provide basic nutrition to pupils. Suspension of the NSNP programme during the pandemic, and the delay in its restoration, was a failure to uphold this duty, and it infringed upon the right of pupils to basic nutrition.
A case was brought to court charging a violation of constitutional and statutory duties and seeking full implementation of the NSNP programme. The court considered the fundamental rights involved, such as the right to education and the right of every child to have basic nutrition.
The court held that the government has a “negative” obligation not to impair a right protected in the Constitution and concluded that the suspension of the NSNP and the delay in restoring it had diminished constitutionally protected rights. The court ruled that all eligible pupils are entitled to a daily meal from the NSNP and ordered restoration of the programme and progress reports on implementation every 15 days.
Source: McBrien J, Rutigliano A, Sticca A. The inclusion of LGBTQI+ students across education systems: an overview. Paris: Organization for Economic Cooperation and Development; 2022 (https://www.oecd-ilibrary.org/education/the-inclusion-of-lgbtqi-students-across-education-systems_91775206-en%3Bjsessionid=Xqg34ZCBv2ts1u3T_j8SBUpOnOPKLJxTA_CALrE_.ip-10-240-5-61).
Mauritius changes the age of paediatrics

In 2021, 13.6% of the population in Mauritius were adolescents (10–19 years of age). Previous surveys among adolescents have shown that additional emphasis on their specific health needs and risky behaviours should be prioritized throughout a broader range of actions addressing such barriers as structural poverty; limited access to adolescent–friendly information, services and education; conservative social norms and discrimination; and insufficient attention to vulnerable and disabled adolescents. Recognizing the essential role and potential of adolescents in society, both for the future of the country and as champions for healthy lifestyles, the Ministry of Health and Wellness (MOHW) is leading the development of the National Strategy for Adolescent Health 2023–2027, with inputs from the Ministry of Education, Tertiary Education, Science and Technology and other ministries, as well as through community engagement.
Providers’ capacity is key for the successful implementation of the strategy. Recently, recognizing the special needs of adolescents, the MOHW has decided to increase the age of paediatrics from 12 years old to 16 years old and to invest in adolescent health training for the country’s paediatricians and policy-makers. With the support of WHO, a master training for a pool of resource persons in providing adolescent-responsive services was organized in April 2023. The two-week training-of-trainers session identified and trained new champions and defenders of adolescent health in Mauritius. Participants learned how to address the multifaceted needs of the adolescent population across key priorities such as mental health, SRH, noncommunicable disease prevention and substance use, among others. This training is an important investment and step in building leadership and providers’ capacity in adolescent health and well-being.
Source: A new national adolescent health strategy in Mauritius. Geneva: World Health Organization; 2023 (https://www.who.int/news/item/22-04-2023-a-new-national-adolescent-health-strategy-in-mauritius).
Ethiopia takes action for long-term solutions for an adolescent-competent workforce

Ethiopia has a rapidly growing population of young people. Those between 15 and 29 years of age make up around one third of a population of 90 million. The Federal Ministry of Health prioritized adolescent health in its Health Sector Transformation Plan (HSTP 2015/16–2019/20) and is committed to being on track to meet the SDG targets by 2030. The National Adolescent and Youth Health Strategy (2016–2020) highlighted the need for strengthening the pre-service training curriculum for adolescent and youth health practitioners. Needs assessment and stakeholder analysis conducted by the Ministry of Health and Regional Health Bureaus, with the support of key development partners, have shown that, although various professionals with short-term orientation trainings are involved in health care service provision for adolescents and youths, access and utilization of health services by adolescents and youths are compromised by a lack of competent providers. Almost all stakeholders identified the lack of competent providers as a major challenge for adolescent and youth health service provision and implementation of the adolescent and youth health strategy. They emphasized that the competency challenges could not be solved by short-term orientation trainings and appreciated the initiative to train adolescent and youth health and development professionals in pre-service training.
Unique contents of the Adolescent Health and Development Curriculum
In addition to basic health professional competencies for all health professionals, the Adolescent Health and Development Curriculum was designed to develop mastery-level competencies in the following:
- normal adolescent development, assessment of adolescent growth and development and identifying and managing developmental disorders;
- age- and developmentally appropriate effective communication with adolescents;
- assessment of adolescent mental health status and management of mental health problems;
- health promotion, risk factors, prevention of risky behaviours, positive developmental interventions, and assessment and management of disorders (substance use disorders, drug use disorders, nutritional disorders, etc.);
- assessment of normative gender issues in the society and implementation of gender-transformative interventions;
- adolescents’ rights to health and effective advocacy to change laws and guidelines that restrict their rights;
- approaches for organization and delivery of quality health care services for adolescents in line with global and national standards;
- engagement and/or participation of adolescents, parents, guardians, community organizations and other sectors in adolescent health and development.
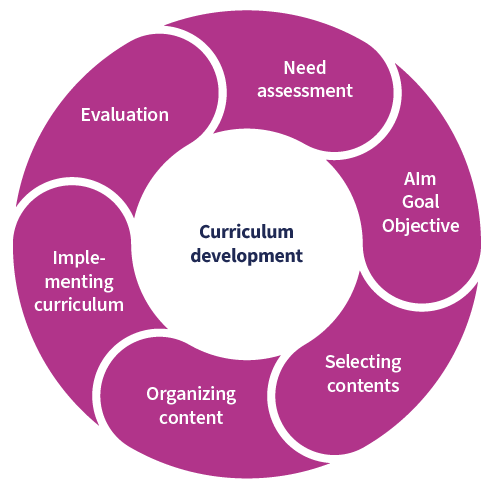
Curriculum development steps and current status
An expert faculty member who taught adolescent reproductive health for about 15 years for Masters of Public Health in Reproductive Health Specialty students initiated development of the curriculum. Then, a team of experts in the school of public health led the overall curriculum development process.
Curriculum development steps and current status
An expert faculty member who taught adolescent reproductive health for about 15 years for Masters of Public Health in Reproductive Health Specialty students initiated development of the curriculum. Then, a team of experts in the school of public health led the overall curriculum development process.
A team of experts has led all curriculum development steps accomplished so far, from needs assessment to setting objectives through developing and organizing contents. To facilitate implementation of the curriculum, the team conducted internal and external curriculum reviews and technically approved the curriculum. It was then ready for implementation. The curriculum is now being used to define competencies and contents for in-service trainings. However, its formal implementation has been delayed. The Human Resources Directorate of the Ministry of Health is completing development of corresponding career paths before graduates enter the health system. A team at the Haramaya University School of Public Health is currently adjusting the curriculum to make it more flexible for admitting both undergraduate and postgraduate students and defining adolescent health competencies for continuous professional development through flexible learning mechanisms (modular, online, self-directed, etc.).
Ensuring that adolescent health is a priority for health professionals: the experience of Uganda

In Uganda around one fifth of the population of 45.7 million is younger than 19 years of age. Yet, as in many African countries, adolescent medicine has not been a recognized specialty, and health care providers receive little adolescent-specific training. This changed after 2016, when faculty from the Makerere University in Kampala – the largest and oldest university in Uganda – attended a capacity building training on adolescent health for countries in east and southern Africa, hosted by the government of Namibia. The training was part of the WHO strategy to support regions and countries to build institutional capacity for adolescent health leadership and training.
After 2016 training for postgraduate students increased, and since 2018 a stand-alone six-week course on adolescent health has been available for second-year residents doing their Master in Paediatrics and Child Health – a significant increase compared with only six hours previously. The course includes lectures, practical training and outreach activities. Postgraduate students who rotate in paediatrics and child health during their six-week placement in the adolescent health and medicine rotation are given the opportunity to undertake school outreach and take care of adolescent patients so that they, too, become champions for adolescent health care.
The next step in Uganda was to increase the availability of adolescent health content in pre-service education and training. It was not a simple process. As a first step, a needs assessment and review of the Bachelor of Medicine, Bachelor of Surgery curriculum showed that key departments, including Paediatrics and Child Health, Nursing, Obstetrics and Gynaecology, and Psychiatry allocated minimal time to adolescent health topics. This finding informed the next step, which was the development of a comprehensive outline of topics for a programme for trainers. Finally, the university conducted a training of faculty and other resource persons to enhance their ability to deliver up-to-date content using interactive teaching techniques. Fifteen master trainers were trained. The undergraduate extracurricular course for medical students, which included 20 hours of training on adolescent health, was launched in June 2019. Since then, over 400 students, including undergraduate and masters students in paediatrics, psychiatry, obstetrics and gynaecology, and public health, have received training in adolescent health.
To equip undergraduate and postgraduate students with practical skills, the Friday Adolescent Clinic and partners has organized practical sessions as part of a biannual skills-building event for adolescents. The Friday Adolescent Clinic opened in May 2013 at the Mulago National Referral Hospital, which is the teaching hospital for the Makerere University College of Health Sciences. The clinic serves as a general adolescent clinic, now providing care for more than 8000 adolescents and young adults. Skills building sessions for adolescents offer a platform for them to come together, learn, share, have fun and learn life skills to enable them to pursue and achieve their goals in life. At the same time, these sessions offer the Master in Paediatrics and Child Health trainees the opportunity to practice building skills among the adolescents.
Source: Internal report from Sabrina Bakeera-Kitaka of the Makerere University College of Health Sciences.
Ghana implements a digital solution to measure the quality of health care services for adolescents

Since 2015 countries have used the Global standards for quality health care services for adolescents developed by WHO and other stakeholders. The aim of the document is to help policy-makers and health service planners improve the quality of health care services so that adolescents find it easier to obtain the health services that they need. In collaboration with stakeholders, WHO proposed eight global standards, focused on adolescent health literacy, community support, an appropriate package of services, provider competencies, facility characteristics, adolescents’ participation, equity and non-discrimination, and data and quality improvements. Periodic monitoring of the implementation of standards was a key component of the document but required time-consuming and expensive surveys. In response, WHO has developed a web-based platform to digitally monitor and evaluate national quality standards. Ghana was among the early adopters to pilot-test the web platform. In 2019 WHO introduced the platform to the Adolescent Health and Development Programme of the Ghana Health Service. Six facilities in the Cape Coast Municipal and Abura Asebu Kwanmankese districts in the Central region were selected for the pilot-test.
The Ghana Health Service provided school nurses with mobile phone tablets and an internet connection to facilitate regular access to the web application. Based on guidance from the global AA-HA! document, the first step in implementation of the web-based platform was adaptation of the global standards for quality health care services to the national context. There followed an orientation of stakeholders on the utility of the web platform. Staff in participating facilities, districts and national focal points were given access to their respective dashboards through specific user accounts. Training sessions on adolescent health and development were held for both trainers and providers. Supervisors visited facilities to support and motivate staff as well as to resolve any ongoing issues. Review meetings at district and national levels provided feedback on project implementation.
After three months of project implementation, six facilities had access to the web platform and had collected information on quality of care from more than 3000 adolescents and health care staff. Staff had been extensively trained in adolescent health and development, and they had adapted the user manual for the web platform to suit local context, including translations into local languages.
Evidence and feedback from Ghana show that the implementation of the web platform has already had a positive impact on the facility, district and national management environment and, importantly, has increased awareness of the unique health needs of adolescents among both health care personnel and adolescents themselves. Improved communication, enhanced professional competencies, standardized tools and materials – such as terms of reference and guidance – have resulted from implementation of the project to date. The country subsequently adopted use of the platform, with support from UNFPA as part of the Joint UN Programme for Adolescent Girls. The number of implementing schools was scaled up to 12 in 2020, 28 in 2021 and 33 in 2022 with support from the UK Foreign, Commonwealth and Development Office through WHO. Plans for 2023 include improving data management for planning, decision-making and advocacy, provision of learning materials to improve school health teaching and learning, sensitization of staff and students in focal schools and training for service providers on the use of the platform.
Source: Internal report from the WHO Adolescent and Youth Health Unit.
Improving adolescent and youth health services in the Democratic Republic of the Congo through collaborative learning

Kinshasa – Nineteen-year-old Armande* recalls her disastrous first visit to a health centre. “It was awful,” says the teen from Kongo Central, in western Democratic Republic of the Congo. “I was younger then and looking for information on HIV, and the nurse there made fun of me in front of everyone because of my age.”
Adolescents face a range of health and societal problems: STIs, including HIV, sexual violence, early and unwanted pregnancy and early marriage.
In the Democratic Republic of the Congo, the government is working to provide access to quality SRH services to adolescents and youth. According to the Strategic Plan for Health and Wellbeing for Adolescents and Youth (2021–2025), one third of the population is between 10 and 24 years of age, but this is a large portion of the population getting little health care: Only 17% of youth and adolescents used health services in 2021.
To improve service quality, WHO has supported the implementation of an innovative collaborative learning project backed by the Global Fund. Service providers work together to identify, discuss and propose solutions for common problems – all while strengthening capacity and developing positive attitudes, which then improve the health services provided to adolescents.
“Young people and adolescents need services that are tailored to them,” says Fidèle Mbadu Muanda, Director of the National Programme of Adolescent Health. “Collaborative learning is about strengthening capacities and changing attitudes among service providers. We’ve aligned the norms and policies linked to youth-oriented health services according to WHO guidance.”
In addition to providing technical guidance for the project, WHO supported trainings and the design of high-quality materials for providers.
The project was launched during 2018 and 2019, covering six districts in the provinces of Western Kasai (Mbuji-Mayi) and Kinshasa. Jeannette Mudipanu, a nurse in Makala’s Saint Clément Hospital Centre who participated in one of the 32 sessions, says she experienced a profound shift in perspective.
“It’s important to understand the individual,” she said. “From there, we must take the time to listen, patiently and without judgement.”
Youth attendance is now up at Saint Clément: Around 600 adolescents visited the centre between July and December 2020, compared with 280 over the same period in the previous year. Exit interviews show a 100% satisfaction rate with the services received.
Based on initial success and lessons learned in the six pilot districts, the project now aims to scale up the collaborative learning approach to 25 zones in five provinces.
* Not her real name.
Source: Adapted from WHO 2022 (544). Improving adolescent and youth health services. Geneva: World Health Organization; 2022 (https://www.afro.who.int/countries/democratic-republic-of-congo/news/improving-adolescent-and-youth-health-services).
France ensures competency-based training of school health doctors

French school health is conceptualized into four complementary components aimed at making school a health-promoting setting: education (life skills, disciplinary competencies), prevention of risks (for example, addictive behaviours, sedentary lifestyles), protection and service (consultations, check-ups). All school staff are expected to contribute to this health promotion dynamic, including school doctors.
In France, as in other European Union countries, the tasks of school doctors are numerous, but they can be summarized in three main blocks:
- individual approach to the health of students: mandatory check-ups at established points (for 6-year-olds to detect learning disorders, at the beginning of secondary school, and for students 16–18 years of age in vocational schools to assess their aptitude to participate in regulated tasks forbidden to minors) and, at any time, interventions for students with special needs or for situations of concern (mainly relating to child protection);
- population approach to the health of students: health education, monitoring of the school environment, training staff on child and adolescent health and well-being and collecting data on the health of students;
- management of health emergencies in the school community: potentially traumatic events, communicable diseases.
Since 1991 school doctors in France are attached to the Ministry of Education. The laws governing their training were last revised in 2007. School doctors graduate from medical school and then must pass a public service competition. For those who are successful, the School of Public Health (École des hautes études en santé publique) provides mandatory training in coordination with the Ministry of Education. Following an interview exploring the candidate’s specialty (usually general practice, paediatrics or public health), their previous career and diploma, an individualized training programme of 8–16 weeks is proposed. Outside the training weeks, the doctors are working autonomously in schools under the supervision of experienced mentors.
A school doctor who is a senior researcher in public health leads the training. The development board, which meet three times a year, ensures the quality of the organization and content of the courses. The board also seeks regular feedback from trainees.
Over the last 15 years, this training has been revised to match the 10 core competencies expected from school doctors and to improve its relevance in a rapidly changing work environment. The competencies are specific and complementary, with no hierarchical order. They are specific to school doctors and are not taught as such in medical school.
The 10 core competencies of French school doctors
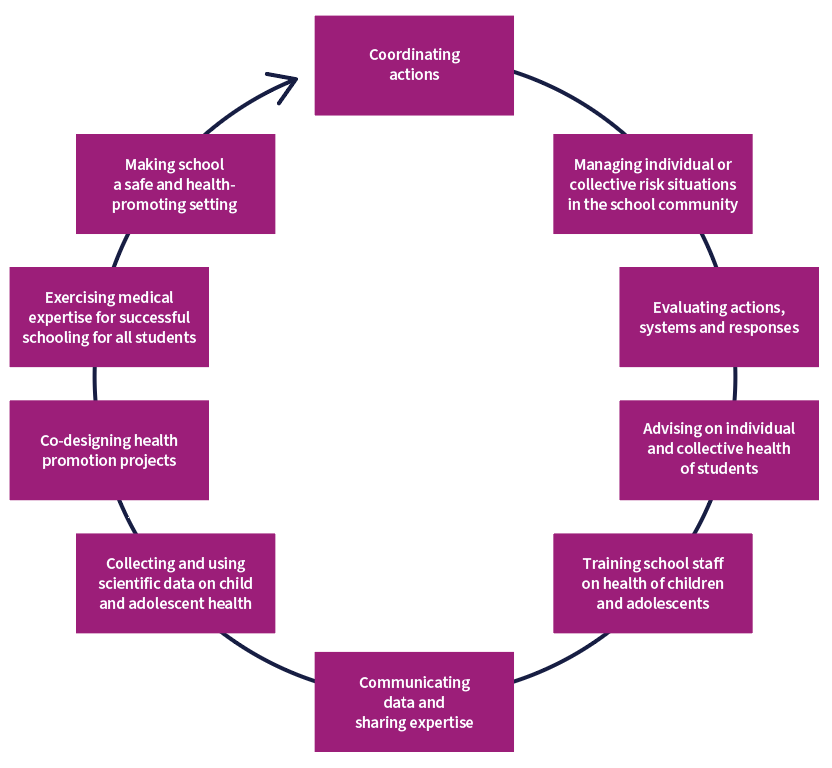
During training, 10 modules nurture these competencies by combining interactive academic teaching face-to-face, distance learning and pragmatic and professional skills developments.
The 10 complementary modules of the training of French school doctors

France, like other countries, faces a shortage of medical doctors. This makes the role of SHS, which have a unique position at the intersection of the health and education systems, even more crucial. Importantly, the training of school doctors must prepare them to change their working paradigm from curing to preventing, from clinical settings to the school as a health setting and from an individual to a collective perspective. In the French system, school doctors are key to ensuring that schools adopt a true health promotion perspective and fight health inequalities. This is to the benefit of the health – and, therefore, the successful learning – of all students.
The Adolescent Girls Initiative – Kenya

The Adolescent Girls Initiative – Kenya (AGI–K) investigated the effect of multisectoral cash-plus interventions addressing the community and households, combined with interventions in the education, health and wealth-creation sectors, on fertility, SRH and education outcomes. The study randomly assigned 2075 girls 11 to 14 years of age to one of four intervention packages:
- community dialogues on unequal gender norms and their consequences (violence prevention)
- violence prevention and cash transfers conditioned on children attending school (education)
- violence prevention, education and health and life skills training (health)
- violence prevention, education, health, financial literacy training and savings activities (wealth).
The interventions were implemented between 2015 and 2017, and participants were followed until 2019. The primary outcomes were fertility (ever had sex, pregnancy or delivery) and HSV-2 infection. Secondary outcomes were violence prevention, education, health knowledge and wealth creation.
The study demonstrated that multisectoral cash-plus interventions for the community and household, combined with interventions in the education, health and wealth-creation sectors, directly benefited individual girls in early adolescence and reinforced protective factors against pregnancy in early adolescence. Such interventions, therefore, potentially have beneficial impacts on the longer-term health and economic outcomes of girls who live in impoverished settings.
Source: Gender and age-responsive social protection: the potential social cash transfers to advance adolescent rights and capabilities. Policy brief No 12. New York: UN Women; 2019 (https://www.unwomen.org/sites/default/files/Headquarters/Attachments/Sections/Library/Publications/2019/UN-Women-Policy-brief-12-Gender-and-age-responsive-social-protection-en.pdf).
Zambia’s National Diversion Framework

The National Diversion Framework was developed by the Ministry of Community Development and Social Services, supported by UNICEF, following an initial assessment of diversion and alternative sentencing practices in Zambia. The assessment found that diversion was being carried out across Zambia in an informal, ad hoc manner, typically by police officers mediating with the accused child and complainant (and their families). It also found that more intensive and rehabilitative “diversion” programmes were being implemented through a number of civil society organizations and NGOs. The vast majority of referrals into these programmes, however, came from the courts and were not strictly diversion, but rather constituted community-based sentencing alternatives. These measures were limited to parts of the country where links had been established to appropriate service providers (notably, Lusaka and Kitwe).
The stakeholders who consulted in the process of developing the framework identified a need for standardization of approaches to diversion and consistency in the implementation of diversionary measures. They generally agreed that a national framework on diversion was needed.
The framework aims to assist all stakeholders, including the law enforcement agencies, social welfare, public prosecutors, magistrates and NGO service providers, to respond to child offences by diversion out of formal court proceedings, in accordance with the UN Convention on the Rights of the Child. The framework sets out the scope, criteria, process and options for the use of diversion in Zambia, such as warnings, restorative measures (mediation, family group/community conferences, restitution) and rehabilitative programmes.
Source: Juvenile justice: national diversion framework. Lusaka: Ministry of Community Development and Social Services; 2018 (https://www.unicef.org/zambia/media/1306/file/Zambia-diversion-framework-2018.pdf).