International Women's Day: When WHO decided to update its guidelines on antenatal care (ANC), there was a feeling that maybe a different approach was needed. The current ANC guidance was based on a set of systematic reviews of the evidence and a trial and it proposed a model with at least four antenatal care visits (also known as focused antenatal care). It has been widely adopted in low- and middle-income countries, yet in 2012, only 52% of pregnant women had four or more ANC visits. To try and understand why this might be and how uptake of antenatal care services could be improved, a set of reviews were undertaken to look at what was missing from current antenatal care programmes.
The traditional approach to providing antenatal care services generally focuses on clinical services – the prevention of potential complications, the assessment or physical risk or ill-health and largely ignores the psychosocial aspects of pregnancy. Some studies, however, have suggested that these other factors might be sufficiently important to women to influence their engagement (or not) with health care services during their pregnancy.
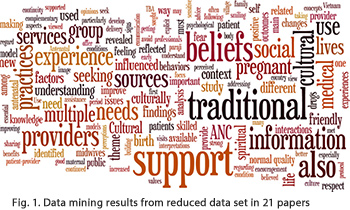 To try and understand what those factors might be and what women want and expect from the antenatal care services, a review was carried out that synthesised the qualitative literature on the subject. The study initially identified over 8000 potential studies but for reasons of quality and relevance, this number was gradually reduced to 38 papers that were subjected to a final analysis. The 38 studies came from countries from all regions of the world with the exception of Australasia.
To try and understand what those factors might be and what women want and expect from the antenatal care services, a review was carried out that synthesised the qualitative literature on the subject. The study initially identified over 8000 potential studies but for reasons of quality and relevance, this number was gradually reduced to 38 papers that were subjected to a final analysis. The 38 studies came from countries from all regions of the world with the exception of Australasia.
Pregnancy should be a positive experience
Not surprisingly, what emerged from the study was that women across countries, cultural groups and varying sociodemographics were looking for a “positive pregnancy experience”. In fact the study suggested that there are four main themes that matter to women (and, by extension, to their partners and families):
- maintaining physical and sociocultural normality;
- maintaining a health pregnancy (including preventing and treating risks, illness and death);
- effective transition to a positive labour and birth;
- achieving positive motherhood (including maternal self-esteem, competence and autonomy).
These themes in turn can be the basis for designing a woman-centred antenatal care service that would include :
- tailored, rather than routine, clinical/therapeutic practices (biomedical tests and interventions, integrated with local practices and knowledge where these are appropriate and effective);
- relevant and timely information (physiological, biomedical, behavioural and sociocultural);
- support (social, cultural, emotional and psychological.
In addition, the data also indicated that the characteristics, attitudes and behaviours of formal and informal care providers are important to pregnant women.
What next?
The findings from this analysis suggest that the design of future antenatal care guidelines and programmes should embrace these non-clinical components not just as general underpinning principles but as interventions that have of equal weight with clinical care. WHO will be adopting this approach as it moves forward with the revision of its antenatal guidelines, to be issued later in 2016. In addition, service providers across all levels and whether working in hospitals or local communities should embrace these concepts and consider how they can work with women, families and communities to provide positive antenatal care experience and ensure optimal uptake of ANC services.
Related links
What matters to women: a systematic scoping review to identify the processes and outcomes on antenatal care provision that are important to healthy pregnant women.
- See journal article
- Quality of care for pregnant women and newborns – The WHO vision.
- Antenatal care for healthy pregnant women: a mapping of interventions from existing guidelines to inform the development of new WHO guidance on antenatal care
