
6.2 National surveys of costs faced by TB patients and their households
The World Health Organization (WHO) End TB Strategy includes the target that no tuberculosis (TB) patients or their households face catastrophic costs (including direct medical expenditures, non-medical expenditures and income losses) because of TB disease. Monitoring of progress towards this target can inform monitoring of progress towards universal health coverage (UHC); however, this target should not be confused or directly compared with the Sustainable Development Goal (SDG) UHC indicator for financial protection from health care expenditures among the general population (Box 6.1.1). WHO has established standard methods for conducting a national survey to assess the direct and indirect costs incurred by people with TB and their households (TB patient cost surveys) (1).
Since 2015, there has been substantial progress in the implementation and planning of national TB patient cost surveys (Fig. 6.2.1). By September 2021, 25 countries had completed a survey: Benin (2018), Brazil (2019), Burkina Faso (2020), China (2016), the Democratic Republic of the Congo (2019), El Salvador (2021), Fiji (2017), Ghana (2016), Indonesia (2020), Kenya (2017), Lao People’s Democratic Republic (2019), Lesotho (2019), Mongolia (2017), Myanmar (2015), Nigeria (2017), Papua New Guinea (2019), the Philippines (2016), Republic of Moldova (2016), Solomon Islands (2019), Thailand (2020), Timor-Leste (2017), Uganda (2018), the United Republic of Tanzania (2019), Viet Nam (2016) and Zimbabwe (2018).
In the 23 surveys for which results have been reported, the percentage of TB patients and their households that experienced catastrophic total costs (defined as >20% of household expenditure or income) ranged from 13% (95% confidence interval [CI]: 10–17%) in El Salvador to 92% (95% CI: 86–97%) in Solomon Islands (Fig 6.2.2). The pooled average for all 23 countries, weighted for each country’s number of notified cases, was 47% (95% CI: 33–61%) (Fig. 6.2.3).
Among 19 countries that reported disaggregated data, the pooled averages were 45% (95% CI: 35–56%) for drug-susceptible TB and 87% (95% CI: 80–93%) for drug-resistant TB (DR-TB) (Fig. 6.2.3). The percentage of TB patients with DR-TB and their households that experienced catastrophic total costs ranged from 50% (95% CI: 14–86%) in Burkina Faso to 100% (95% CI: 92–100%) in Uganda.
The distribution of costs varied among countries (Fig. 6.2.4) but it was evident that – despite the widespread norm of “free TB care” policies – TB-affected households still face direct medical costs. Such costs accounted for a sizeable proportion of total costs in some countries (e.g. 19% in both Ghana and Mongolia). Minimizing direct medical costs borne by TB patients should be a high priority for national TB programmes (NTPs) and ministries of health.
The surveys also showed that actions are needed to eliminate non-medical costs and to reduce income losses. The combined cost of transportation, food, nutritional supplements and other non-medical expenditures (“direct non-medical costs”) accounted for a substantial share of total costs in some countries, including Solomon Islands (80%), Fiji (73%), Kenya (64%), Uganda (60%), El Salvador (58%), Timor-Leste (53%), and the United Republic of Tanzania (51%).
Income losses associated with loss of employment or time lost while seeking or staying in care accounted for the largest single share of total costs in Burkina Faso (77%), Brazil (65%), Papua New Guinea (59%), Mongolia (57%), Lesotho (50%), Myanmar (48%), Nigeria (47%) and Viet Nam (44%).
All cost categories are influenced by the model of TB care; for example, to what extent there is reliance on hospitalization or outpatient care, the frequency with which attendance at health facilities is requested and the level to which services are decentralized to bring the services close to the community. They are also influenced by ease of access to the health facilities used to provide care.
Further details of individual national surveys are available elsewhere (2–8). In addition, WHO, in collaboration with national survey teams, is currently preparing a publication that will provide full details about the results and policy implications of the national TB patient cost surveys completed in 2016–2020. This book is due to be published in early 2022.
Fig. 6.2.1 National surveys of costs faced by TB patients and their households since 2015: progress and plans (as of September 2021)
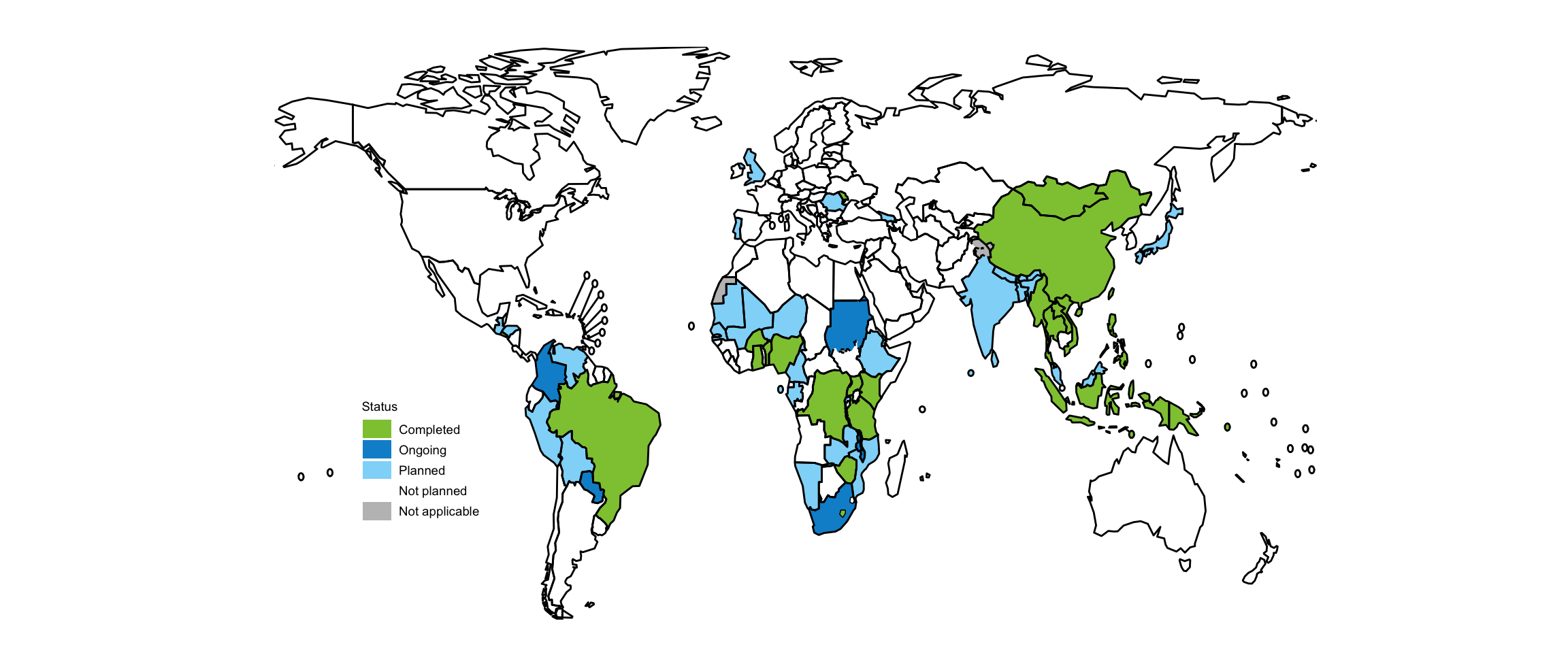
Fig. 6.2.2 Estimates of the percentage of TB patients and their households facing catastrophic costs, national surveysa implemented 2016–2020

Source: WHO Global TB Programme
Fig. 6.2.3 Average percentage of people with TB and their households facing catastrophic costs in 24 national surveys completed since 2015
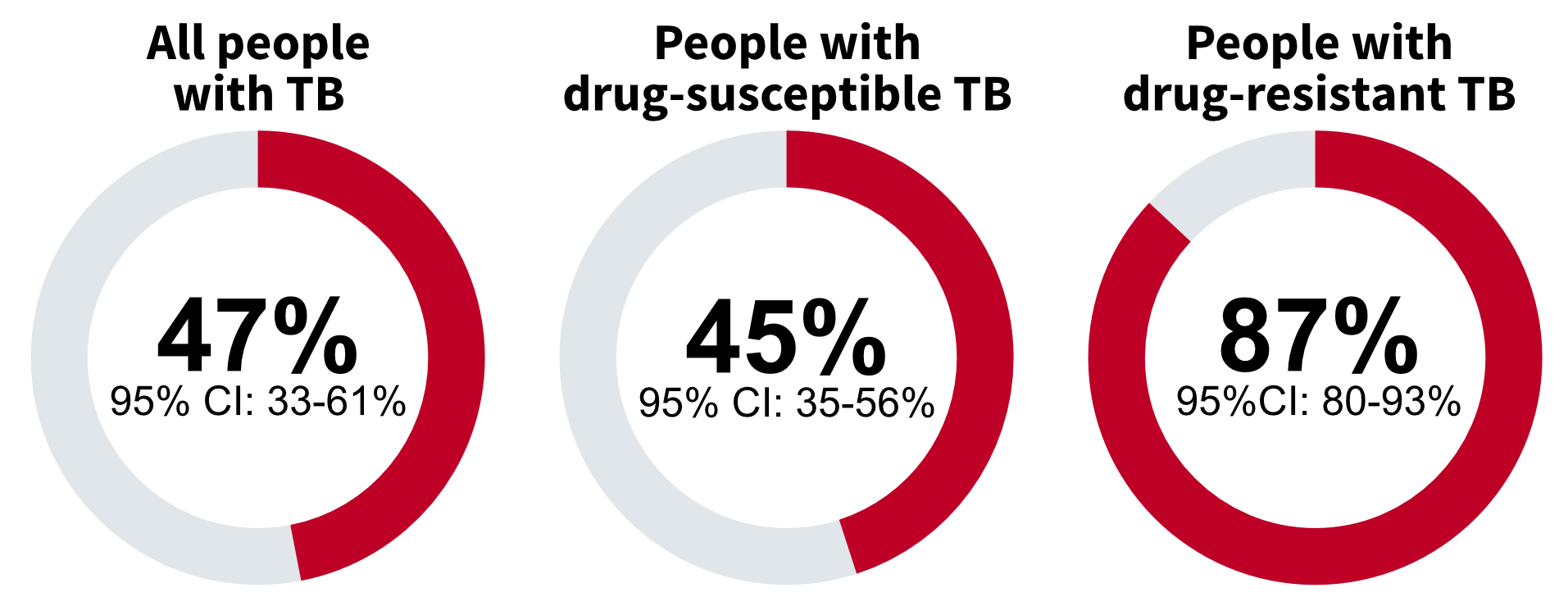
Fig. 6.2.4 Distribution of costs faced by TB patients and their households in 21 national surveys completed 2016–2020

- Tuberculosis patient cost surveys: a handbook. Geneva: World Health Organization; 2017 (https://www.who.int/publications/i/item/9789241513524).
- Pedrazzoli D, Siroka A, Boccia D, Bonsu F, Nartey K, Houben R, Borghi J. How affordable is TB care? Findings from a nationwide TB patient cost survey in Ghana. Trop Med Int Health. 2018. 23(8):870–878.
- Nhung NV, Hoa NB, Anh NT, Anh LTN, Siroka A, Lonnroth K, Garcia Baena I: Measuring catastrophic costs due to tuberculosis in Viet Nam. Int J Tuberc Lung Dis. 2018;22(9):983–90.
- Viney K, Amaral S, Marques EB, Siroka A, Lopes C, Nery SV. Four of five tuberculosis patients experience catastrophic costs related to TB diagnosis and care in Timor-Leste. Int J Tuberc Lung Dis 2019;23(11):1191–7.
- Chittamany P, Yamanaka T, Suthepmany S, Sorsavanh T, Siphanthong P, Sebert J et al. First national tuberculosis patient cost survey in Lao People’s Democratic Republic: assessment of the financial burden faced by TB-affected households and the comparisons by drug-resistance and HIV status. PLOS One. 2020;15(11):e0241862.
- Muttamba W, Tumwebaze R, Mugenyi L, Batte C, Sekibira R, Nkolo A et al. Households experiencing catastrophic costs due to tuberculosis in Uganda: magnitude and cost drivers. BMC Public Health 2020;20:1409.
- Pedrazzoli D, Carter DJ, Borghi J, Laokri S, Boccia D, Houben RM. Does Ghana’s National Health Insurance Scheme provide financial protection to tuberculosis patients and their households? Soc Sci Med 2021;277:113875.
- Kaswa M, Minga G, Nkiere N, Mingiedi B, Eloko G, Nguhiu P, Baena IG. The economic burden of TB-affected households in DR Congo. Int J Tuberc Lung Dis. 2021 Nov 1;25(11):923-932.
