COVID-19 Global Risk Assessment- Version 9
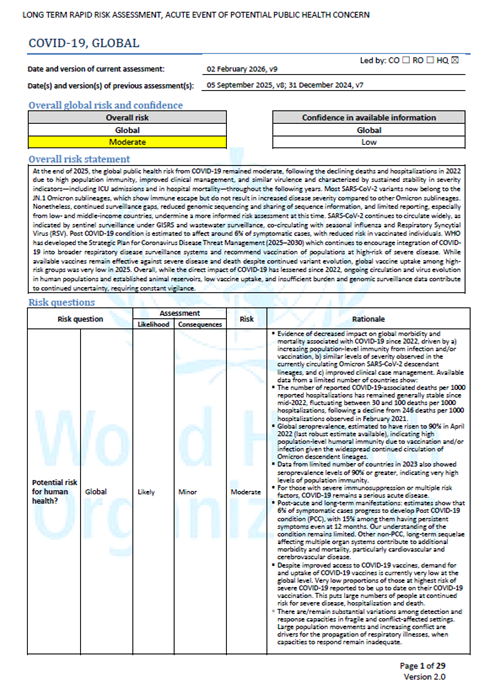
Overview
WHO regularly conducts risk assessments for graded emergencies in accordance with the WHO Emergency Response Framework. Since January 2020, WHO conducted global risk assessments for COVID-19 every three months. With the lifting of the public health emergency of international concern, WHO has shifted to producing COVID-19 risk assessments every six months.
At the end of 2025, the global public health risk from COVID-19 remained moderate, following the declining deaths and hospitalizations in 2022 due to high population immunity, improved clinical management, and similar virulence and characterized by sustained stability in severity indicators—including ICU admissions and in hospital mortality—throughout the following years. Most SARS-CoV-2 variants now belong to the JN.1 Omicron sublineages, which show immune escape but do not result in increased disease severity compared to other Omicron sublineages. Nonetheless, continued surveillance gaps, reduced genomic sequencing and sharing of sequence information, and limited reporting, especially from low- and middle-income countries, undermine a more informed risk assessment at this time. SARS-CoV-2 continues to circulate widely, as indicated by sentinel surveillance under GISRS and wastewater surveillance, co-circulating with seasonal influenza and Respiratory Syncytial Virus (RSV). Post COVID-19 condition is estimated to affect around 6% of symptomatic cases, with reduced risk in vaccinated individuals. WHO has developed the Strategic Plan for Coronavirus Disease Threat Management (2025–2030) which continues to encourage integration of COVID-19 into broader respiratory disease surveillance systems and recommend vaccination of populations at high-risk of severe disease. While available vaccines remain effective against severe disease and death despite continued variant evolution, global vaccine uptake among high-risk groups was very low in 2025. Overall, while the direct impact of COVID-19 has lessened since 2022, ongoing circulation and virus evolution in human populations and established animal reservoirs, low vaccine uptake, and insufficient burden and genomic surveillance data contribute to continued uncertainty, requiring constant vigilance.
