
Tuberculosis-related innovations during the COVID-19 pandemic
The disruptions to health care caused by the coronavirus (COVID-19) pandemic have triggered a wave of creativity among tuberculosis (TB) programmes intent on maintaining essential services for their patients. The global TB reports of 2020 (1) and 2021 (2) highlighted the impact of such initiatives since early on in the pandemic, based on national reporting and literature. Starting in late 2020, the World Health Organization (WHO) invited countries and partners to send brief descriptions of innovations introduced to address different challenges posed by the pandemic. These experiences were compiled in two reports that were released in May 2021 and April 2022 (3, 4).
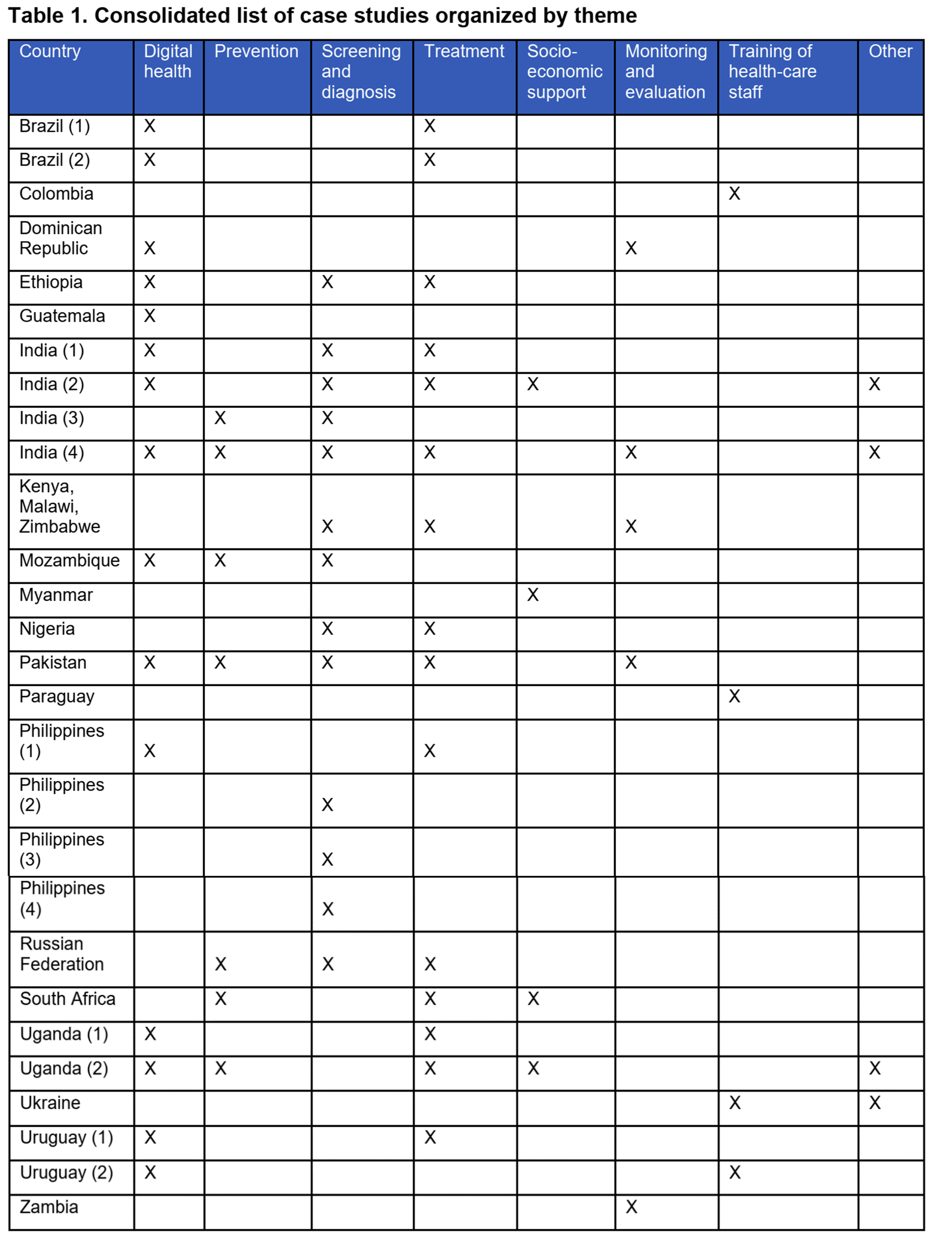
The two reports bring together 29 case studies provided by national health authorities, nongovernmental organizations and academic groups working in 20 countries worldwide (Table 1). About half of these reports describe the use of digital technologies for different functions in TB care; for example, electronic recording and reporting, digital adherence, eLearning, telemedicine and conditional cash transfers mediated electronically.
One of the new strategies implemented by countries to diagnose more people with TB and COVID-19 has been dual (“bidirectional”) testing. This involves testing a person for both TB and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) based on their risk for both diseases. Three approaches are used: concurrent testing for TB or SARS-CoV-2 in people who may have either condition at presentation, testing for TB disease in people with confirmed COVID-19 and testing for SARS-CoV-2 in people with confirmed TB disease. The testing yield has varied widely between countries that reported findings from these approaches, given differences in the criteria applied for choosing who to screen, acceptance of complete testing by individuals targeted and the level of community transmission of SARS-CoV-2 in those tested. Hence, there are concerns that dual testing could misdirect case-finding efforts, waste resources and widen gaps in case detection even further, thus forgoing higher yield activities.
WHO collaborated with the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund) and other partners to advise countries on how best to implement dual testing (5). A survey of dual-testing activities was also coordinated by WARN/CARN-TB - a network of national TB programmes (NTPs) in West and Central Africa - supported by the Special Programme for Research and Training in Tropical Diseases (TDR) and WHO, between May and August 2022. In total, 32 countries located across all six WHO regions participated in this survey (6); findings from the survey included the following:
- TB was diagnosed in 0.7–4.5% of people tested concurrently for both TB and SARS-CoV-2 at presentation in four countries;
- TB was detected in 0.03% and 1% of confirmed COVID-19 patients tested for TB in two countries; and
- SARS-CoV-2 positivity in people with confirmed TB disease was 0.1–13.9% in four countries reporting data.
These findings suggest that, in most countries, the yield of TB testing in confirmed or presumptive COVID-19 patients was higher than the 0.5% TB prevalence that WHO recommends as the threshold for population-level TB screening. The variation in testing efficacy might be explained by variations in the prevalence of TB in the places where SARS-CoV-2 was tested and in the criteria used for selecting people to be tested for TB. SARS-CoV-2 positivity among people with confirmed or presumptive TB was likely to be influenced by the pattern of transmission and the stage of the pandemic in each setting.
The case studies collected by WHO represent a small sample of a much bigger effort to maintain TB services worldwide. Starting in 2020, over 100 countries are now reporting provisional TB data to WHO at a monthly or quarterly frequency, providing a better picture of the critical functions of case management and data reporting at NTP level; an example for Zambia is shown in Fig. 1.
Summaries of six case studies reported to WHO that illustrate various innovations to address disruptions to TB programmes caused by the COVID-19 pandemic are provided below. Further details are available elsewhere (3, 4).
Colombia
Colombia developed eLearning for community leaders and virtual supervision as two components of a multipronged TB care strategy during the pandemic, alongside measures to enhance infection control, drug supply and molecular diagnostics. More than 1000 health workers were trained virtually, and the programme has maintained the continuity of services, including for people with drug-resistant TB (DR-TB).
Kenya, Malawi and Zimbabwe
A project coordinated by the International Union Against Tuberculosis and Lung Disease (UNION) in Kenya, Malawi and Zimbabwe explored how the electronic reporting of monthly data allowed the timely assessment of treatment progress in TB patients. The study was run in 36 health care facilities (18 in Nairobi, Kenya; 8 in Lilongwe, Malawi; and 10 in Harare, Zimbabwe). In collaboration with NTPs, data were collected electronically every month from the selected health facilities. The TB treatment outcomes of monthly cohorts of patients enrolled on treatment 8 months previously were used. Monthly reports, including a narrative explaining changes and observed interventions, were prepared and shared each month with the national authorities. Overall numbers of people presenting with presumptive pulmonary TB decreased (country range: 31–46% decrease). In all countries, TB treatment success was less severely affected and most of the decline appeared to be due to missing information on final outcomes.
The Philippines
In the Philippines, treatment success rates among patients with rifampicin-resistant TB (RR-TB) remains unsatisfactory (in 2019, only 67% of patients started treatment). This situation is largely attributed to a high proportion of patients who are lost to follow-up because of adverse drug reactions. In March 2020, the NTP adopted the shorter all-oral bedaquiline-containing regimen, shortly after WHO announced its new recommendation on this regimen. In addition to being shorter, this regimen is also less toxic than previously used alternatives and eliminates the need for daily injections. By the end of the year, 1466 patients with RR-TB had started this new treatment, representing about one quarter of the RR-TB cases starting treatment in the country in 2020. Nonetheless, overall treatment success was 73% – noticeably higher in this annual cohort than in previous years.
Uganda
During the COVID-19 pandemic, digital adherence technologies were used as part of patient-centred delivery of TB preventive treatment (3 months of weekly rifapentine and isoniazid) in people with HIV at a clinic in the capital, Kampala. The study assessed the effect on acceptance and treatment completion. Participants were assigned to in-person observation (with interactive appointment reminders to visit the clinic) or self-administered therapy (with interactive voice reminders and adverse-event check-ins). Voice reminders were in the most widely spoken local language. Although the study has yet to finish, remote monitoring of treatment adherence has shown promising results that could help reduce clinic congestion and travel costs. Most patients enrolled found the weekly interactive dosing and appointment reminders helpful.
Zambia
In Zambia, national notifications of TB cases fell in the early phases of the pandemic. The national TB and leprosy programme introduced weekly surveillance of key performance indicators of TB services – including notifications of both drug-susceptible TB and DR-TB, and the availability of medicines and diagnostics – to better understand the extent of disruptions at national, provincial and district levels. Interactive, virtual discussions were set up for this purpose. High-performing districts and provinces were able to share best practices with others, and low-performing districts shared their challenges and identified the necessary support. All the districts implemented best practices in case finding, and notifications started to recover thereafter (Fig. 1).
Fig. 1 Provisionala number of monthly TB case notifications in Zambia, 2020–2022
References
Global tuberculosis report 2020. Geneva: World Health Organization; 2020 (https://www.who.int/publications/i/item/9789240013131).
Global tuberculosis report 2021. Geneva: World Health Organization; 2021 (https://www.who.int/publications/i/item/9789240037021).
Programmatic innovations to address challenges in tuberculosis prevention and care during the COVID-19 pandemic. Geneva: World Health Organization; 2021 (https://www.who.int/publications/i/item/9789240037021).
Consolidated report of country success stories in mitigating the impact of the COVID-19 pandemic on TB services. Geneva: World Health Organization; 2022 (https://apps.who.int/iris/bitstream/handle/10665/353334/9789240048232-eng.pdf).
Testing for both tuberculosis and SARS-CoV-2. Geneva: Global Fund to Fight AIDS, Tuberculosis and Malaria; 202 (https://www.theglobalfund.org/media/11438/covid19_tb-testing_briefingnote_en.pdf).
Dual testing for tuberculosis and SARS-CoV-2: country reports. 2022: WARN/CARN-TB (https://tdr.who.int/docs/librariesprovider10/meeting-reports/dual-testing-for-tb-and-sars-cov-2-country-reports.pdf).
