
2.4 Drug-resistant TB: treatment enrolment, coverage and outcomes
People with drug-resistant TB (DR-TB) need treatment with regimens that include second-line drugs, such as bedaquiline and fluoroquinolones (1). WHO recommends different regimens for rifampicin-resistant TB (RR-TB) or multidrug-resistant TB (MDR-TB, defined as resistance to both rifampicin and isoniazid); isoniazid-resistant TB; pre-extensively drug-resistant TB (pre-XDR-TB, defined as TB that is resistant to rifampicin and any fluoroquinolone) and XDR-TB (resistance to rifampicin, any fluoroquinolone and at least one of bedaquiline or linezolid). These regimens are more expensive (≥US$ 1000 per person) and cause more adverse events than first-line treatments for drug-susceptible TB.
Globally in 2022, 175 650 people were enrolled on treatment for MDR/RR-TB. This was a small increase from 161 843 in 2021 (+8.5%) and 150 510 in 2020 (+17%), but still below 181 533 in 2019. Most of those enrolled on treatment were people aged ≥15 years (Fig. 2.4.1).
Trends in treatment enrolment between 2010 and 2022 vary considerably among the 30 high MDR/RR-TB burden countries (Fig. 2.4.2).
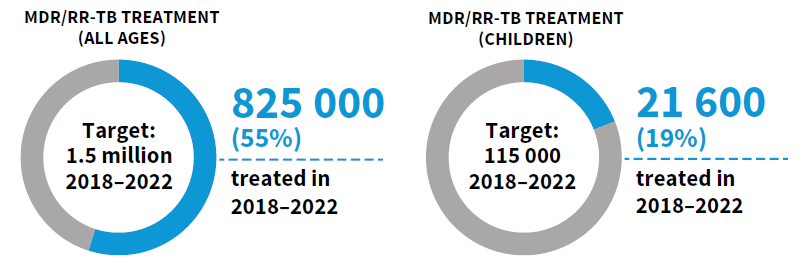
Globally, the cumulative total number of people reported as enrolled on treatment for MDR/RR-TB from 2018 to 2022 was 824 988, only 55% of the 5-year target (2018–2022) of 1.5 million that was set at the UN high-level meeting on TB in 2018. For people aged 0–14 years specifically, the cumulative number was 21 625, only 19% of the 5-year target of 115 000.
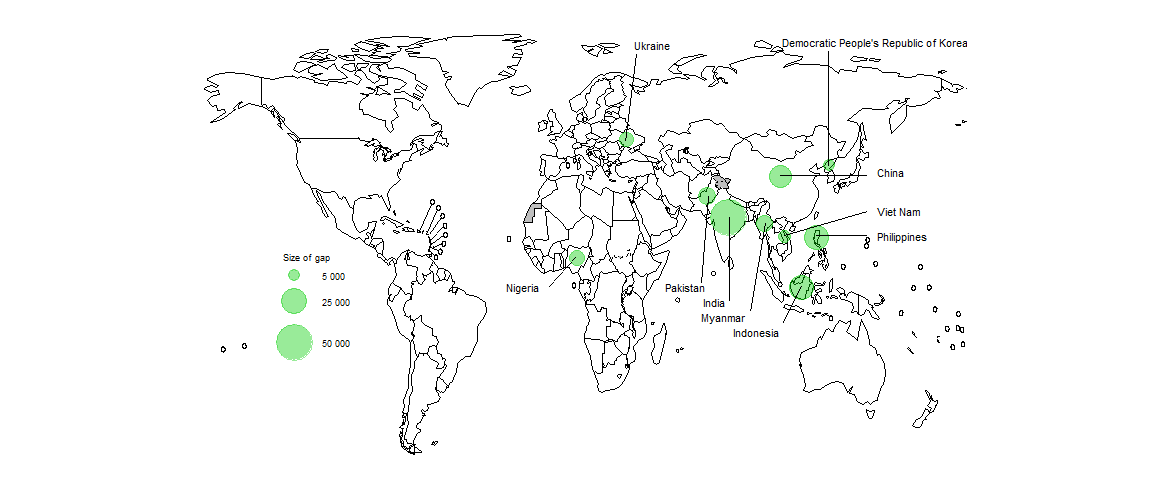
The numbers of people being detected with MDR/RR-TB and enrolled on treatment fall far short of the estimated number of people developing MDR/RR-TB (incident cases) each year (Fig. 2.4.4). Closing the gap requires improvements in overall detection of people with TB (Section 2.3), improvements in the percentage of those diagnosed with TB who are bacteriologically confirmed (necessary to test for drug resistance) and improvements in the coverage of testing for RR-TB (Section 2.2).
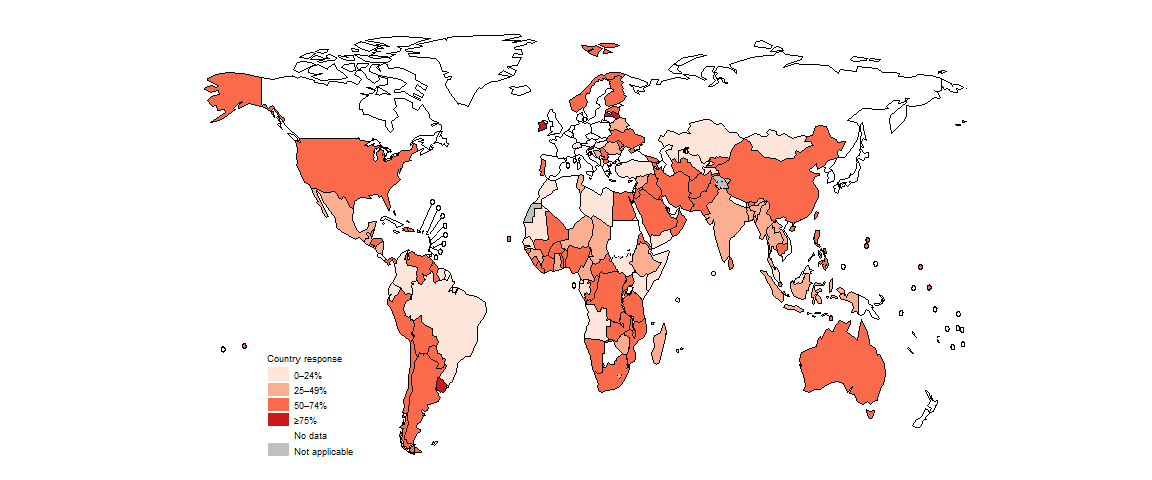
Estimated levels of treatment coverage for MDR/RR-TB in 2022, approximated as the number of people enrolled on treatment for MDR-TB in 2022 divided by the estimated number of people who developed MDR/RR-TB (incident cases) in 2022 and expressed as a percentage, remain low: globally, 43% in 2022 (Fig. 2.4.5). The WHO regions with the highest levels of treatment coverage are the African Region and the Region of the Americas. Among the 30 high MDR/RR-TB burden countries, only eight had treatment coverage levels of ≥50% in 2022: Azerbaijan, Belarus, India, Kazakhstan, Peru, the Republic of Moldova, the Russian Federation and South Africa. Those with particularly low levels (<20%) included the Democratic People’s Republic of Korea, Myanmar, Somalia and Zambia.
In 2022, 10 countries accounted for 70% of the global gap between the estimated number of people who developed MDR/RR-TB and the number of people enrolled on treatment for MDR/RR-TB (Fig. 2.4.6).
Globally in 2020 (the latest patient cohort for which data are available), the success rate for people treated for MDR/RR-TB was 63%; this was an improvement from 60% in 2021 and up from 50% in 2012 (Fig. 2.4.7).
Among WHO regions, the treatment success rate in 2020 was lowest in the European Region and highest in the Eastern Mediterranean Region (Fig. 2.4.8).
Since 2018, WHO has recommended all-oral regimens for the treatment of MDR/RR-TB, marking a major advance compared with previously-recommended regimens that included injectable agents (1). The latest guidelines, updated in 2022, include three major categories of regimen (2). The first is a short 6-month all-oral regimen (which may be extended for up to 3 months if necessary) consisting of bedaquiline (B), pretomanid (Pa), linezolid (L) and moxifloxacin (M), referred to as BPaLM (for people with pre-XDR-TB, the regimen can be used without moxifloxacin and is referred to as BPaL). The second category is all-oral short regimens of 9 months (which may be extended for up to 2 months if necessary). The third category is longer regimens of 18–20 months that may include an injectable drug (amikacin). The short 6-month regimen is prioritized for use and is recommended for people aged 14 years and older who have MDR/RR-TB or pre-XDR-TB.
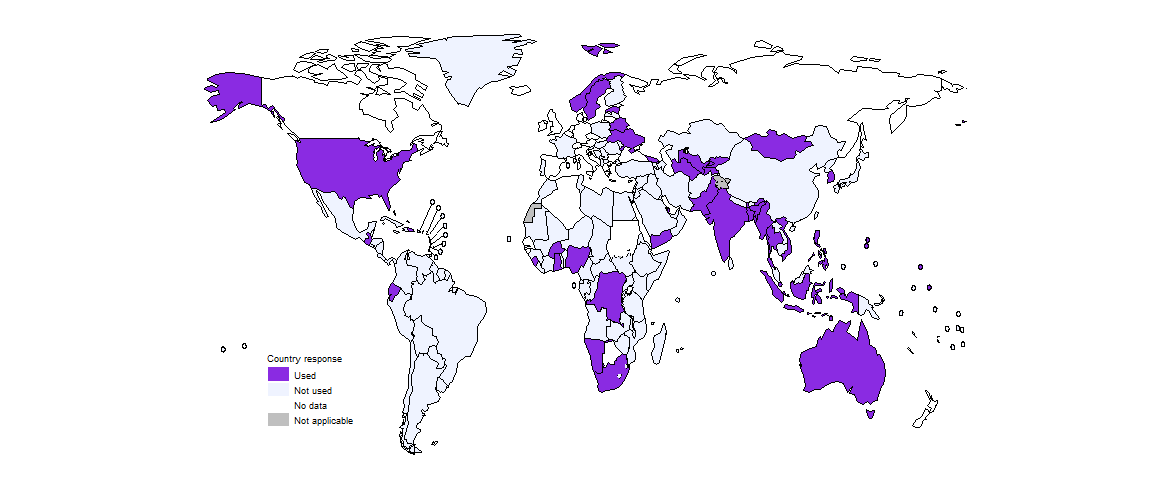
By the end of 2022, 40 countries had started to use the BPaLM/BPaL regimens for the treatment of MDR/RR-TB or pre-XDR-TB (Fig. 2.4.9). In 2022, 1745 people with MDR/RR-TB were reported to have been started on the BPaLM/BPaL regimens.
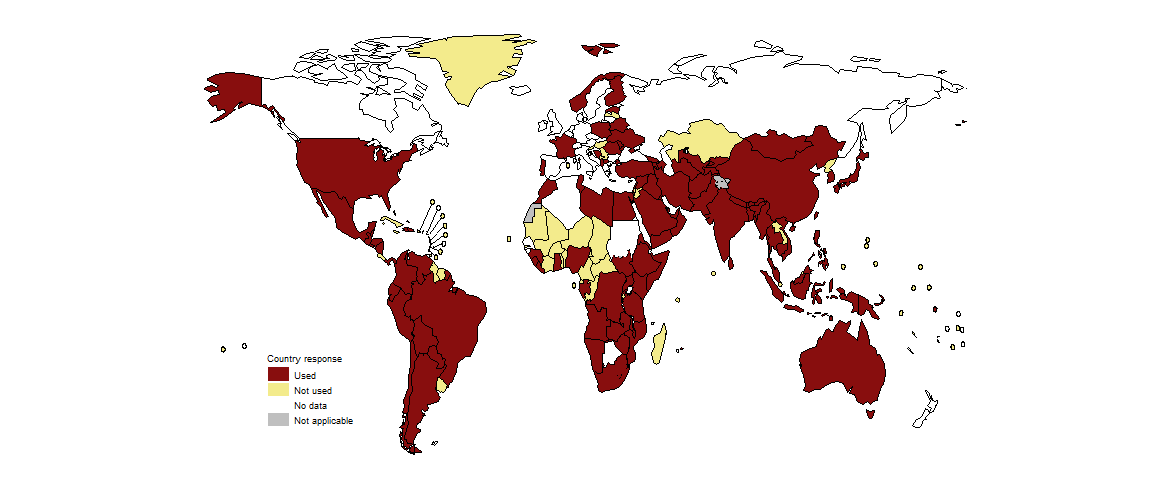
By the end of 2022, 92 countries were using the shorter 9-month regimens for the treatment of MDR/RR-TB (Fig. 2.4.10). This was similar to the level of 93 in 2021, and up from 65 in 2020.
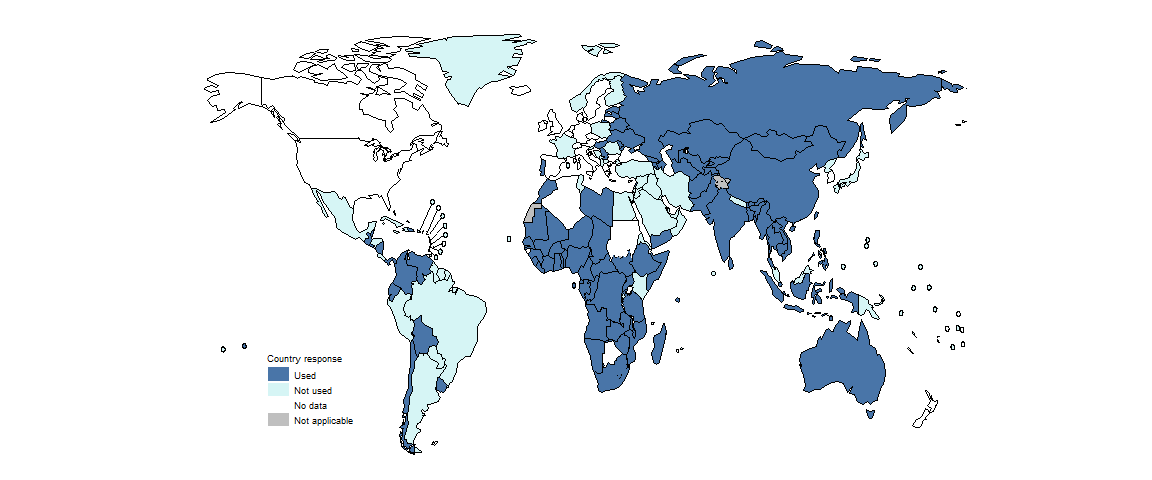
At the end of 2022, 105 countries were using the longer regimens of 18–20 months for the treatment of MDR/RR-TB (Fig. 2.4.11). This was higher than in 2020 (92) but a reduction from 109 in 2021.
In 2022, at least some people diagnosed with drug-resistant TB were being monitored for adverse events in most countries (Fig. 2.4.12).
Further country-specific details about treatment for drug-resistant TB are available in the Global tuberculosis report app and country profiles.
Further details about the BPaLM/BPaL regimen are provided in one of the report’s featured topics.
References
Rapid сommunication: key changes to treatment of multidrug- and rifampicin-resistant tuberculosis (MDR/RR-TB). Geneva: World Health Organization; 2018 (https://iris.who.int/handle/10665/275383).
WHO consolidated guidelines on tuberculosis, Module 4: Treatment – drug-resistant tuberculosis treatment, 2022 update. Geneva: World Health Organization; 2022 (https://iris.who.int/handle/10665/365308).
