- Implementation of the Global Influenza Strategy (2019-2030):
In 2024, Member States (MS) in the Region continued influenza preparedness in the context of implementation of the WHO Global Influenza Strategy (2019–2030) and Pandemic Influenza Preparedness (PIP framework) in alignment with the International Health Regulations (IHR) (2005). WHO’s coordinated efforts for synergies between influenza preparedness and pandemic response capacity-building were targeting achieving two high-level outcomes as outlined in the Global influenza strategy: (1) Ensuring availability of better global tools for prevention, detection, control, and treatment of influenza and (2) Building stronger country capacities through evidence-based influenza programmes established on the principle of universal coverage that meets national health security needs.
To support efforts in building pandemic response capacity, the WHO Health Emergencies (WHE) Programme at SEARO has played a key role in enhancing influenza pandemic response systems through investments under the Pandemic influenza preparedness framework. SEARO provided leadership in planning the implementation of the new six-year Pandemic influenza preparedness framework: partnership contribution high-level implementation plan III 2024-2030 in the region. In collaboration with the PIP Partnership Contribution (PC) Secretariat, SEARO prioritized countries for receiving PC funds during the first biennium of the HLIP-III (2024-30). In addition to the seven eligible countries from HLIP-II (India, Nepal, Bangladesh, Timor-Leste, Indonesia, Myanmar, and DPR Korea), three more countries—Maldives, Sri Lanka, and Bhutan—were prioritized for funding under HLIP-III.

Figure 1: The scope of the Global Influenza Strategy 2019-30.
To contribute to the achievement of the Sustainable Development Goals (SDGs) through WHO's General Programme of Work, the WHE/SEARO coordinated strategic leadership with Member States (MS) in the South-East Asia Region (SEAR) to advance these goals via the strategic objectives outlined in the Global Influenza Strategy.
In alignment with the proposed shift towards an expanded Global Influenza Surveillance and Response System, the strategic objective of "Surveillance, Monitoring, and Data Utilization" in the Global Influenza Strategy was actively supported by WHE/SEARO. The region continued to advocate for and provide technical support for the implementation of integrated sentinel surveillance systems for influenza and other respiratory viruses with epidemic and pandemic potential, with a primary focus on integrating influenza and SARS-CoV-2 to Influenza Like Illness (ILI) / Severe Acute Respiratory Infection (SARI) sentinel surveillance.
Additionally, WHE facilitated Phase-III of WHO’s pilot project for integrating Respiratory Syncytial Virus (RSV) surveillance into the existing Influenza Like Illness (ILI) and Severe Acute Respiratory Infection (SARI) sentinel surveillance network. Building on the progress of Phase-II, which involved India, Nepal, and Thailand, WHE/SEARO prioritized additionally Sri Lanka, Bhutan, and Bangladesh for technical and logistical support during Phase-III.
While SEARO’s concerted efforts focused on supporting Member States (MS) to consolidate the integration of influenza and SARS-CoV-2 to Influenza Like Illness (ILI) / Severe Acute Respiratory Infection (SARI) sentinel surveillance, the RSV surveillance component aimed to identify needs and coordinate policy, strategic, and technical support for establishing and sustaining RSV surveillance within integrated ILI/SARI sentinel surveillance. This initiative seeks to generate evidence for decision-making regarding the introduction of RSV vaccines and the use of monoclonal antibodies within the expanded Global Influenza Surveillance and Response System (GISRS) Network.
To provide policy and strategic guidance and to better streamline upstream activities related to the operational implementation of the Global Influenza Strategy at the country level, the WHO Regional Office for South-East Asia (SEARO), in collaboration with the WHO Regional Office for the Western Pacific (WPRO), conducted the "Seventeenth Bi-regional Meeting of National Influenza Centres (NICs) and Influenza Surveillance in the WHO South-East Asia and Western Pacific Regions" in Manila, Philippines, from 20-22 November 2024.
The meeting focused on (1) Reviewing the progress made and challenges encountered in influenza and respiratory pathogen surveillance across the two WHO regions between August 2023 and July 2024, including potential implications for enhancing preparedness for future influenza and respiratory pathogen pandemics. (2) Gathering Inputs from Member States for (a) strengthening existing integrated, laboratory-assisted influenza and respiratory virus surveillance systems., (b) Using new epidemiological, surveillance, and laboratory diagnostic approaches for the early detection of novel influenza, avian influenza, and other respiratory pathogens through an integrated surveillance approach, leveraging the expanded GISRS. (3) Discussing approaches for the implementation, strengthening, and sustainability of surveillance systems for seasonal, zoonotic, and pandemic influenza, as well as other epidemic respiratory diseases in the two regions.
In addition, on 19th November, prior to the bi-regional meeting, WHE SEARO conducted the Annual South-East Asia Regional Meeting on operational planning for the implementation of the Global Influenza Strategy and preparedness for other respiratory viruses in 2025 in SEAR.
Participants shared progress on integrated influenza and other priority respiratory pathogen surveillance, defined programmatic and laboratory priorities, and described the outcomes of the joint national and international Surveillance Reviews conducted in 2024. They agreed on actionable steps for: (a) improving the performance of integrated sentinel surveillance of Influenza Like Illness (ILI) and Severe Acute Respiratory Infections (SARI); (b) enhancing readiness through National Influenza Pandemic Preparedness Plans (NIPPPs); and (c) better implementing regional resilient strategies, such as genomic sequencing of respiratory pathogens through the NICs. Participants recommended strengthening the community of practice of the expanded GISRS in SEAR through: (a) knowledge sharing; (b) aligning national and regional efforts with the global influenza strategy and other initiatives; and (c) jointly establishing priorities for 2025 and beyond to support coordinated activities for preparedness and resilience for influenza and other respiratory viruses.

Figure 2: Participants of the "Seventeenth Bi-regional Meeting of National Influenza Centres (NICs) and Influenza Surveillance in the WHO South-East Asia and Western Pacific Regions" in Manila, Philippines, from 20-22 November 2024. (Photo-WHO/WPRO)
To support the achievement of the strategic objective of 'Pandemic Preparedness and Response' in the Global Influenza Strategy through strengthening influenza-related IHR core capacities in the Southeast Asia Region (SEAR), the annual review meeting for the implementation of the Pandemic Influenza Preparedness (PIP) Partnership Contributions (PC) in SEAR was held in New Delhi, India, from 15 to 16 October 2024. The aim of the meeting was to review the implementation of the first year of the PIP PC biennium work plan (2024–2025) under HLIP-III, identify issues and challenges, and develop recommendations for improved implementation in 2025 in fund-recipient Member States (MS) in the region. This was done alongside the implementation of the monitoring and evaluation framework and reporting milestones.
The two-day meeting provided an opportunity for PIP PC recipient countries to share updates on their implementation, best practices, key issues, challenges, and plans for 2025. During the review, the PIP Secretariat presented the operational framework of HLIP-III, the monitoring and evaluation framework highlighting global gains and achievements, and financial updates.
Member States and other participants agreed on a set of recommendations to enhance and accelerate the implementation of the PIP Partnership Contributions in the region, aiming to strengthen collaborative efforts in improving the core capacities required for pandemic influenza preparedness.
Under the strategic objective of “Surveillance, monitoring and data utilization” in the Global Influenza Strategy multiple efforts have been made by WHO, WHO Collaborating Centres and other partners to support MS to adhere to the threshold of processing at least 50 samples and preferably 150 samples per week for diagnosis of Influenza and SARS CoV 2 at the national level as recommended in the “WHO End-to-end integration of SARS-CoV-2 and influenza sentinel surveillance: revised interim guidance” and recently published Implementing the integrated sentinel surveillance of influenza and other respiratory viruses of epidemic and pandemic potential by the Global Influenza Surveillance and Response System.
The number of specimens processed for testing for influenza (and SARS-CoV-2) in the South-East Asia Region (SEAR) Member States by the end of week 49 in 2024 was 55,357 samples (median: 1,174.5). This represents a 2.5% increase in the number of specimens processed in 2024 compared to the same period in 2023 (53,975 samples; median: 1,194). The total number of samples processed in all SEAR countries in 2024 was 32% less than the expected number of 80,850 samples to be processed over 49 weeks, based on the national threshold of 150 samples per National Influenza Centre (NIC) per week. However, for operational feasibility, WHO recommends that at least 50 samples be processed per week, as stated in the 'WHO End-to-End Integration of SARS-CoV-2 and Influenza Sentinel Surveillance: Revised Interim Guidance.' When this recommendation was applied, the number of samples processed for influenza (and SARS-CoV-2) testing over 49 weeks was 1.1 times higher than the minimum expected number of 26,950 samples for the region.
The trend of samples processed for testing for influenza (and simultaneously for SARS-CoV-2) with multiplex real-time reverse transcription polymerase chain reaction (rt-PCR) assays for the period from 2022 to 2024 is given in figure 4.
Except in 2022, the region as a whole managed to process respiratory specimens well above the regional target of 550 samples per a week. In 2024 there was a declining trend from 17 weeks and it is in line with the overall linear declining trend towards the end of the year. However, the difference in 2024 was that the number of samples processed in 47 to 49 weeks were well below the regional target of 550 per week.
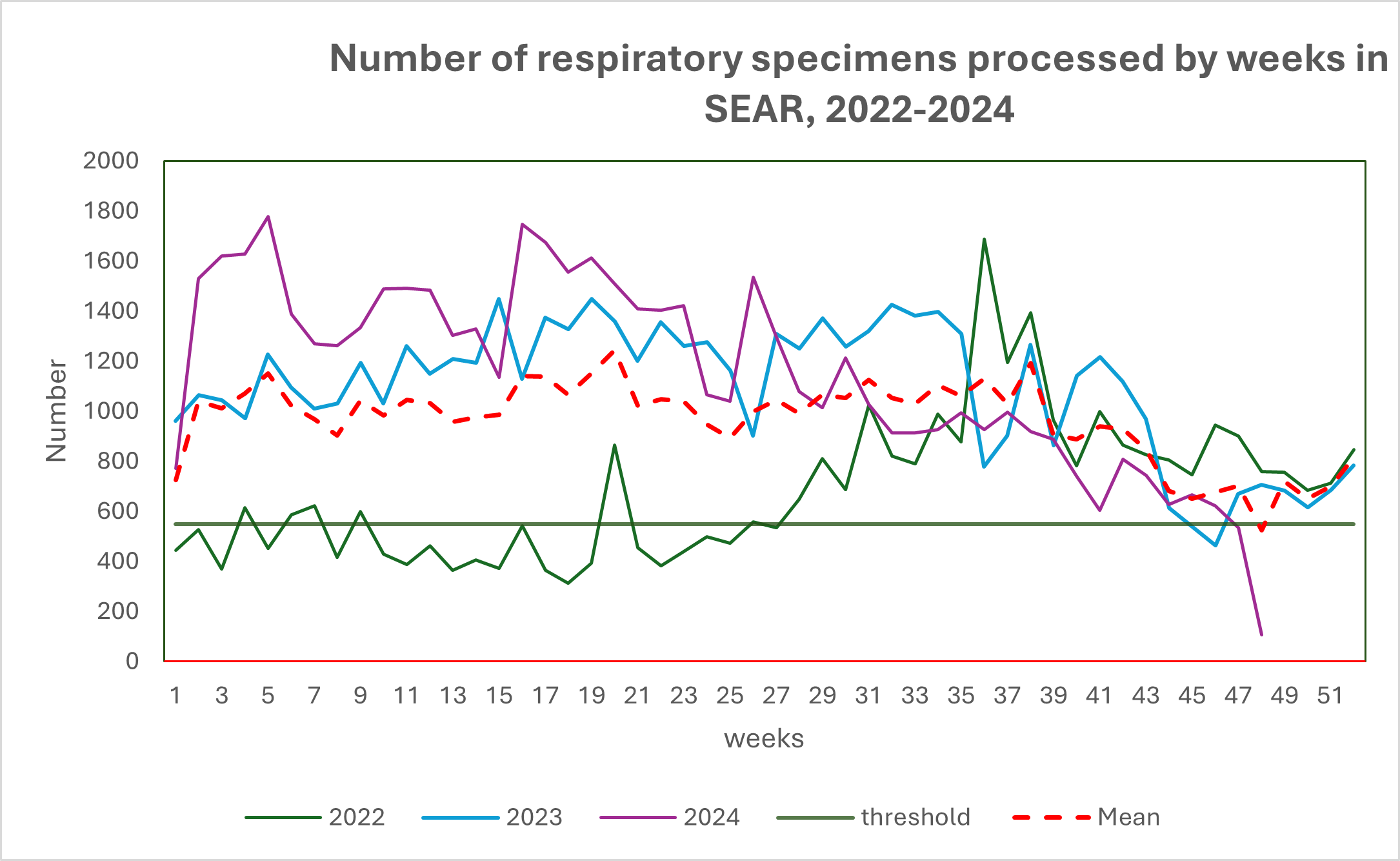 Figure 3: Number of sentinel surveillance specimens processed for testing for Influenza and SARS CoV 2 by weeks and years in WHO South-East Asia Region, 2022-2023. (Source-Flu Net WHO)
Figure 3: Number of sentinel surveillance specimens processed for testing for Influenza and SARS CoV 2 by weeks and years in WHO South-East Asia Region, 2022-2023. (Source-Flu Net WHO)To provide guidance to Member States in reducing the seasonal influenza burden and its health and societal impact, the Regional Office continued to analyze the transmission patterns and characteristics of circulating seasonal influenza types and subtypes. The transmission patterns of seasonal influenza varied from country to country and even within different geographical regions of large countries.
In 2024, while the virus was transmitted year-round, the region observed a unimodal transmission pattern of the seasonal influenza virus.
The peak of transmission in 2024, indicated by 21% positive specimens for influenza, was observed in the 25th week. The seasonal influenza virus continued its transmission consistently throughout the year, with the percentage of positive specimens ranging from 1.9% to 21%. This variability in transmission across different countries in the region reflects the heterogeneous nature of transmission periods, as shown in the cumulative regional transmission dynamics. Country-specific transmission patterns are available at Influenza laboratory surveillance information .
In 2024, influenza type A predominated circulation followed by Influenza Type B(Victoria) and influenza type B (un-subtyped). (Figure 5)
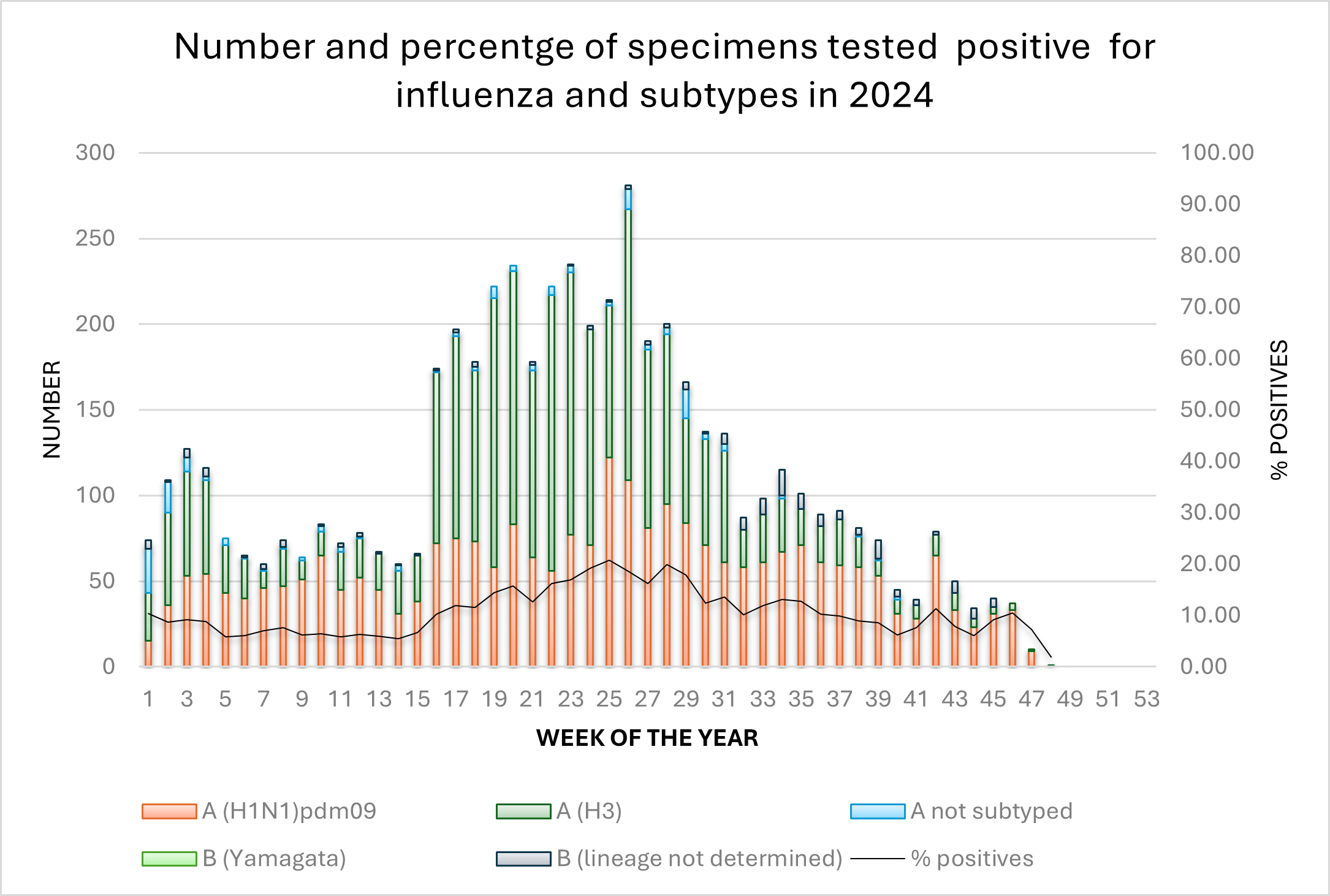 Figure 4: Number and percentage of specimens positive for influenza by subtype in the South-East Asia Region in 2024. (Source: Flu Net, WHO)
Figure 4: Number and percentage of specimens positive for influenza by subtype in the South-East Asia Region in 2024. (Source: Flu Net, WHO)As per the recommendations of the 'WHO End-to-end Integration of SARS-CoV-2 and Influenza Sentinel Surveillance: Revised Interim Guidance,' nine countries in the region (excluding the Democratic People's Republic of Korea and Myanmar) regularly reported SARS-CoV-2 detection results through samples tested in their integrated ILI/SARI sentinel surveillance systems to the WHO global data reporting platform (RespiMART). The results for the region are summarized in figure 6.
The samples collected through the sentinel surveillance system, based on ILI and SARI case definitions, tested positive for SARS-CoV-2 throughout the year. The proportion of samples that tested positive ranged from 9.7% in the 21st week to 0.9% in the 39th week of the year.
South-East Asia Region-specific influenza surveillance information is available at Influenza surveillance outputs
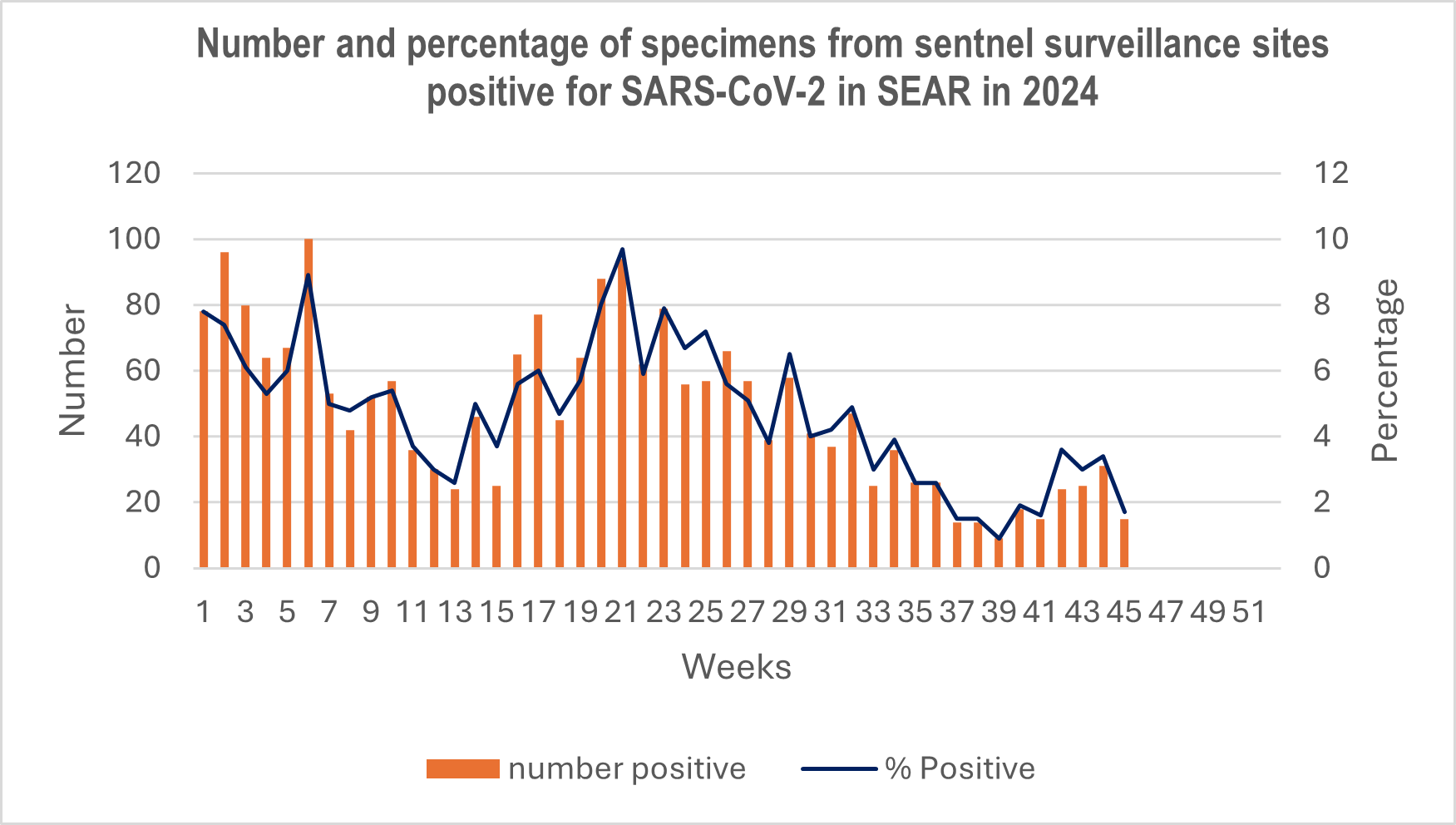 Figure 5: Number and percentage of specimens from sentinel surveillance sites positive for SARS-CoV-2 in the South-East Asia Region in 2024 (Source: Flu Net, WHO)
Figure 5: Number and percentage of specimens from sentinel surveillance sites positive for SARS-CoV-2 in the South-East Asia Region in 2024 (Source: Flu Net, WHO)WHE contributed to building stronger country capacities, which is one of the high-level outcomes of the Global Influenza Strategy in 2024.
To build stronger country capacity in 'Surveillance, Monitoring, and Data Utilization,' a strategic objective of the Global Influenza Strategy, WHE conducted a joint national and international influenza surveillance review, as well as a training on influenza data management, analysis, and Pandemic Influenza Severity Assessment in Indonesia (Figure 7 & 8). Both activities were supported by influenza experts from the Ministries of Health of Indonesia, Bangladesh, Nepal, Sri Lanka, and India, Rajarata University of Sri Lanka, the United States Centers for Disease Control and Prevention (US CDC), and the Victoria Infectious Disease Reference Laboratory (VIDRL) in Melbourne, Australia.

Figure 6: National and international experts reviewed the ILI/SARI sentinel surveillance system and the public health laboratory in Indonesia from 29th July to 2nd August 2024. (Photo-IHM/WHE/SEARO)

Figure 7: National and international experts conducted the training on influenza data management, analysis and Pandemic Influenza Severity Assessment(PISA) in Jakarta, Indonesia on 22-26 July 2024. (Photo-IHM/WHE/SEARO)
To advance the assessment of every influenza epidemic, including pandemics, the WHE programme strengthened country capacities in the South-East Asia Region (SEAR) for pandemic influenza severity assessment (PISA) through influenza surveillance, monitoring, and data utilization. In collaboration with the Global Influenza Programme, WHE/SEARO introduced The updated WHO pandemic influenza severity assessment (PISA) guide in India to support efforts in the country. Bangladesh and Bhutan adopted a different approach by conducting two national PISA training workshops, with the participation of a PISA consultant from WHO’s Global Influenza Programme. Additionally, WHE facilitated a series of webinars for Indonesia, which culminated in a hands-on classroom training session in Jakarta, along with influenza data management and analysis training, held from 22–26 July.
By the end of 2023, all 11 Member States (MS) in the region had successfully established National Influenza Centres (NICs), formally recognized by the World Health Organization (WHO). This achievement reflects the enhanced capacity of these countries to respond to influenza threats. To further strengthen the NICs' capabilities, the WHO's Health Emergencies (WHE) programme, in collaboration with the Global Influenza Programme, introduced the revised Terms of Reference (ToR) for NICs. As part of this initiative, Nepal, Thailand, and Bangladesh participated in the pilot phase to implement these revised ToR.
To maintain the quality of influenza testing at the National Influenza Centres (NICs), the Health Emergencies (WHE) programme continued to support the participation of NICs from the region in the External Quality Assurance Programme (EQAP) for Influenza, organized by the Global Influenza Programme (GIP). A total of ten Member States took part in the programme, with all 10 countries achieving a perfect score of 100% for both seasonal and non-seasonal influenza virus panels.
PIP partnership contributions were invested in supporting laboratory capacity strengthening in the area of influenza and other respiratory pathogens of pandemic potential. In this regard, to advance the laboratory biosafety agenda at National Influenza Centres (NICs) in the South-East Asia Region (SEAR) within the Global Influenza Surveillance and Response System (GISRS), the Infectious Hazard Management Unit and Public Health Laboratory Scientist (PHLS) at WHE/SEARO, in collaboration with the Global Influenza Programme, supported NICs and other stakeholders in the Maldives, Nepal and Sri Lanka in conducting Infectious Substances Shipping Training.
With a forward-looking approach to incorporating Respiratory Syncytial Virus (RSV) surveillance into the expanded Global Influenza Surveillance and Response System (GISRS), the Health Emergencies (WHE) programme strengthened capacities in generating evidence on RSV through pilot projects in Nepal, Thailand, and India as part of Phase 2 of the WHO’S RSV surveillance initiative in 2024. In addition to the countries involved in Phase II, WHE facilitated the inclusion of Bangladesh, Sri Lanka, and Bhutan in Phase III of the RSV surveillance initiative, scheduled to begin in 2025.
In response to a request from the Ministry of Health of Bhutan, WHO organized a mission from 24–28 June 2024 to support the establishment of RSV surveillance in Bhutan. The mission included experts from the Global Influenza Programme, WHE/SEARO, and the WHO Collaborating Centre (WHO CC) for Reference and Research in Melbourne, Australia. The team reviewed Bhutan’s national operational plan for integrating RSV into the ILI/SARI sentinel surveillance system and assessed the capacity of laboratory and sentinel sites to conduct RSV surveillance.
Zoonotic influenza poses significant risks to public health and the global economy. Proactive measures, including early detection, surveillance, and public health interventions, are crucial to mitigating these risks and preventing widespread health and economic losses. Recognizing these impacts, "Minimizing zoonotic influenza risk" has been outlined as a key control goal in the Global Influenza Strategy. To effectively minimize this risk, decision-makers must identify the primary transmission mechanisms and pinpoint the geographical areas where outbreaks are most likely to occur.
In this regard, as outlined in the Regional Roadmap for Results and Resilience, capitalizing on innovations and advancements in technology, research, and best practices, the IHM unit developed the High Threat Pathogens (HTP) Distribution Assessment and Ranking System (HDARS). HDARS is a suitability mapping tool designed to identify areas highly susceptible to exposure to HTP transmission across multiple interfaces and to assess the significance of associated risk factors. This geospatial operational framework serves as a spatial decision support system, providing guidance to countries in formulating comprehensive surveillance programs and informing targeted, effective interventions to strengthen epidemic and pandemic preparedness strategies for HTPs.
Placing WHO as an enabler, the organization supported Nepal in adapting HDARS for Zoonotic Influenza. Through a country-led process, Nepal successfully applied the tool to support cross-sectoral, risk-based surveillance at the national level ( Development of a zoonotic influenza distribution assessment and ranking system (ZIDAR): Technical application in Nepal to support cross-sectoral risk-based surveillance ). Following a successful in-country technical application and endorsement by the national One Health Committee, the tool is now being planned for rollout at the sub-national level. Aligning with the control goals outlined in the Global Influenza Strategy, WHE is now engaging with other Member States for the implementation of ZIDAR/HDARS across the WHO region, strengthening surveillance capacity for zoonotic influenza and high-threat pathogens within the broader International Health Regulations framework.
Another strategic focus in the Global Influenza Strategy that WHE has concentrated on is "research and innovation." Many Member States in the region are behind in introducing and sustaining seasonal influenza vaccines. Therefore, it is crucial to understand the factors preventing these Member States from making decisions to introduce seasonal influenza vaccines into national programs. To address this, WHO conducted a literature review and performed key informant interviews (KIIs) to identify the enablers and barriers to national seasonal influenza vaccination policymaking and implementation in the WHO Southeast Asia Region. Additionally, WHO conducted a comprehensive analysis of the epidemiological and virological status of seasonal influenza in the region as reported to WHO’s global data-sharing platform by the Member States in SEAR, to assist regional policymaking efforts and the development of evidence-based strategies.
Under the strategic objective of Pandemic Preparedness and Response in the Global Influenza Strategy, WHE continued the work initiated in 2022 on strengthening medical oxygen systems and their management in the context of preparedness for influenza and other respiratory pathogen pandemics. To supplement the medical oxygen infrastructure developed by Member States in WHO’s South-East Asia Region, WHO-SEARO, in collaboration with PATH India, developed two high-quality and reliable knowledge products to strengthen the biomedical capacity for oxygen and respiratory care devices in the region.
Implementation of the Influenza Pandemic Preparedness framework:
To refine WHO's leadership and performance, WHE, together with country offices, planned and implemented the 2024-25 biennium work plan for Pandemic Influenza Preparedness under the new High-Level Implementation Plan (HLIP-III) for 2023-30.
While WHE overall managed the PIP partnership contribution project, fund recipient countries played a key role in leading the implementation of Output 1 (Policy and Plans) and Output 2 (Collaborative Surveillance through GISRs) in the region.
Output 3 (Community Protection) was managed by the Country Preparedness and IHR Unit of WHE. For Output 4 (Regulatory Systems), the regulatory preparedness component was implemented by the UHC/Health Systems Department, while the Immunization and Vaccine Development (IVD) Unit of the UHC/Communicable Diseases Department supported the optimization of plans for effective and efficient deployment of pandemic vaccines within pandemic influenza supplies
The close coordination and collaboration across all three levels of the organization and within departments of the regional office facilitated the effective implementation of the Pandemic Influenza Preparedness Framework. This approach incorporated lessons learned from the COVID-19 pandemic and was aligned with broader global and regional policies
- WHO SEARO leadership and performance in launching Preparedness and Resilience for Emerging Threats (PRET) initiative in WHO South East Asia Region
Launched in April 2023, WHO’s Preparedness and Resilience for Emerging Threats (PRET) initiative is an innovative approach to enhance preparedness and ensure a more equitable and robust response to pandemics. It incorporates the latest tools and approaches for shared learning and collective actions developed during the COVID-19 pandemic and other recent public health emergencies.
Recognizing the importance of the PRET initiative in alignment with the Regional Strategic Roadmap for Health Security and Health System Resilience for Emergencies 2023-2027, WHE-SEARO launched a PRET regional road map. During the Regional workshop on WHO’s Preparedness and Resilience for Emerging Threats (PRET) framework to introduce the Preparedness and Resilience for Emerging Threats Module 1: Planning for respiratory pathogen pandemics in October 2023, Member States (MS) from the region recommended that WHO conduct a regional PRET simulation exercise in 2024, leveraging WHO’s Health Emergency Preparedness, Response and Resilience (HEPR) framework.
In response to the MS request, as a part of the regional road map, from 17 to 18 October 2024, WHE/SEARO along with WHO’s PRET secretariat - conducted a multi-country simulation exercise in New Delhi, India. The exercise focused on planning for respiratory pathogen pandemics, leveraging global, standardized simulation exercise tools to assist country participants to effectively prepare. The exercise objectives were to strengthen regional capacity in pandemic planning, test and evaluate multilateral coordination and communication mechanisms, reinforce and clarify roles and responsibilities among countries and international stakeholders, and identify opportunities for improving cross-border preparedness and collaboration for respiratory pathogen pandemic preparedness and response.
WHO’s “Exercise panPRET-2” simulation scenario was utilized, engaging a group of experts in respiratory pathogens and national pandemic planning from Member States in SEAR along with global Advisory Group members of the Pandemic Influenza Preparedness framework, and development partners.
Participants identified key strengths and gaps in their current national influenza pandemic preparedness plans (NIPPPs), to adapt them into comprehensive respiratory pathogen pandemic plans capable of responding to future pandemics caused by novel respiratory pathogens. Countries outlined their next steps and the support needed from WHO and partners to conduct similar exercises at the national level. These exercises, involving a wider range of stakeholders, are expected to be held before, during, or after the finalization of their national respiratory pathogen pandemic plans using the PRET approach.
 Figure 8: A group of experts in respiratory pathogens and national pandemic planning from Member States, along with Advisory Group members of the Pandemic Influenza Preparedness Framework and development partners, participated in a multi-country simulation exercise using WHO’s Exercise panPRET-2. (Photo -IHM/WHE/SEARO)
Figure 8: A group of experts in respiratory pathogens and national pandemic planning from Member States, along with Advisory Group members of the Pandemic Influenza Preparedness Framework and development partners, participated in a multi-country simulation exercise using WHO’s Exercise panPRET-2. (Photo -IHM/WHE/SEARO)
