Situation at a glance
Description of the situation
In 2025, the global cholera situation continues to pose a significant public health challenge across multiple regions.
Between 1 January and 17 August 2025, a total of 409 222 cholera/AWD cases and 4738 deaths were reported globally, from 31 countries.[1] During the same period in 2024, 510 638 cases and 3248 deaths were reported from 28 countries, representing a 20% decrease in cases, but a 46% increase in deaths.
In 2025, the Eastern Mediterranean Region recorded the highest number of cholera/AWD cases (230 991 cases, six countries), followed by the African Region (172 750 cases, 23 countries), the South-East Asia Region (2985 cholera/AWD cases, five countries), and the Region of the Americas (2496 cases, one country). Cholera-related deaths were highest in the African Region (3763 deaths, CFR 2.2 %), followed by the Eastern Mediterranean Region (943 deaths, CFR 0.4%), the Region of the Americas (31 deaths, CFR 1.2%), and the South-East Asia Region (One death, CFR 0.03%). Meanwhile, the European and Western Pacific regions have not reported any outbreaks.
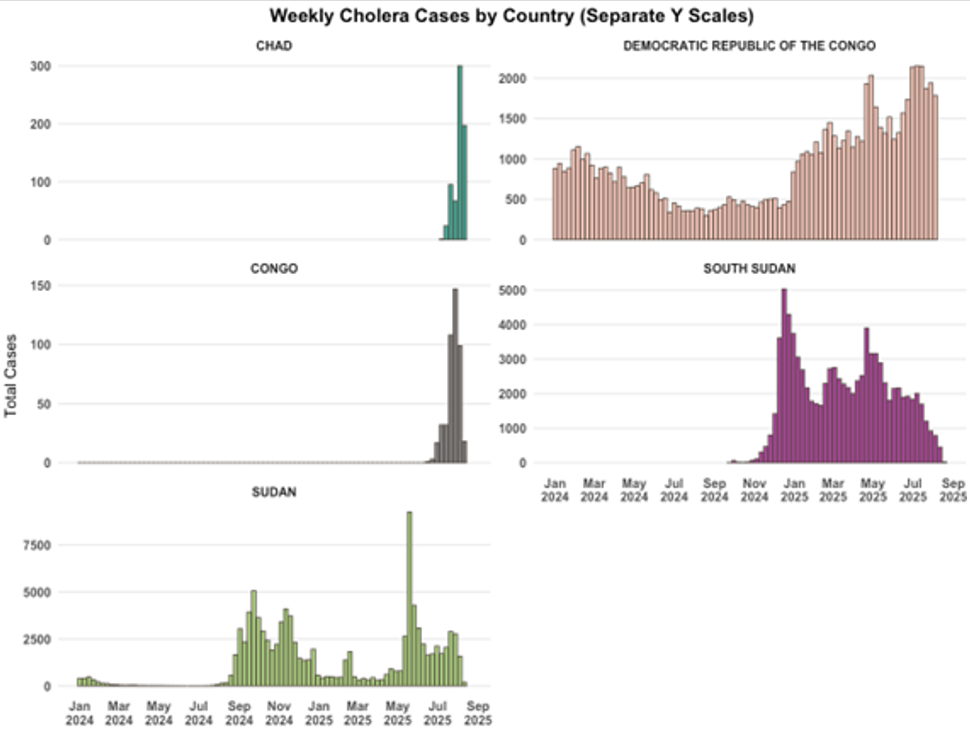
Cholera is resurging in a number of countries, with some that had not reported substantial case numbers in years, including Chad and the Republic of the Congo, while others, including the Democratic Republic of the Congo (DRC), South Sudan, and Sudan, are experiencing outbreaks that are continuing from 2024, with significant geographic expansion. The spread into previously unaffected areas is complicating containment efforts and straining fragile health systems. These trends reveal deep systemic weaknesses in health systems, Water, Hygiene, and Sanitation (WASH), and disease surveillance systems, especially in countries facing humanitarian crises. Cross-border transmission is occurring, underscoring the urgent need for stronger surveillance, timely reporting, and coordinated response across international borders.
The disease burden remains high, particularly in the following countries currently experiencing acute outbreaks: Chad, DRC, the Republic of the Congo, South Sudan, and Sudan. These countries continue to report high transmission rates, case fatality rates, and experience significant challenges in outbreak control and access to care.
However, differences in case definitions and reporting systems have been observed across countries and regions, which may affect the comparability of data and the interpretation of trends. Therefore, given these complexities, the data presented here likely underestimates the true burden of cholera and should be interpreted with caution.
Figure 1. The global cholera and acute watery diarrhoea (AWD) cases per 100 000 population, 1 January to 17 August 2025 *
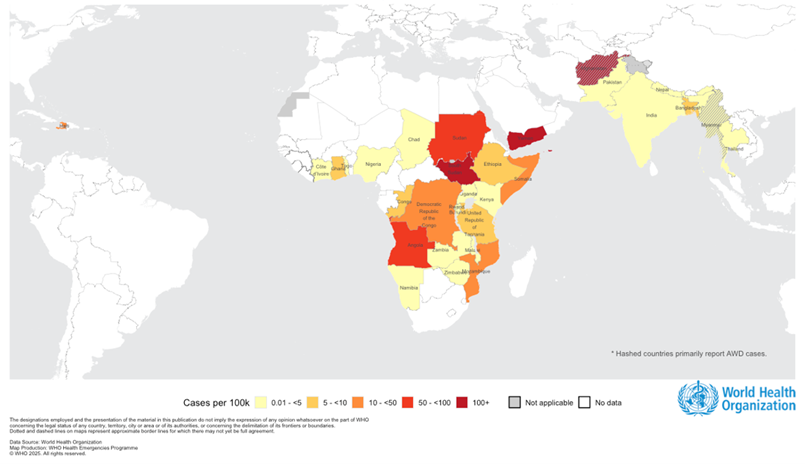
* Afghanistan and Myanmar report AWD cases.
Figure 2. Number of cholera cases by epidemiological week of reporting, as of 17 August 2025. Data source: WHO
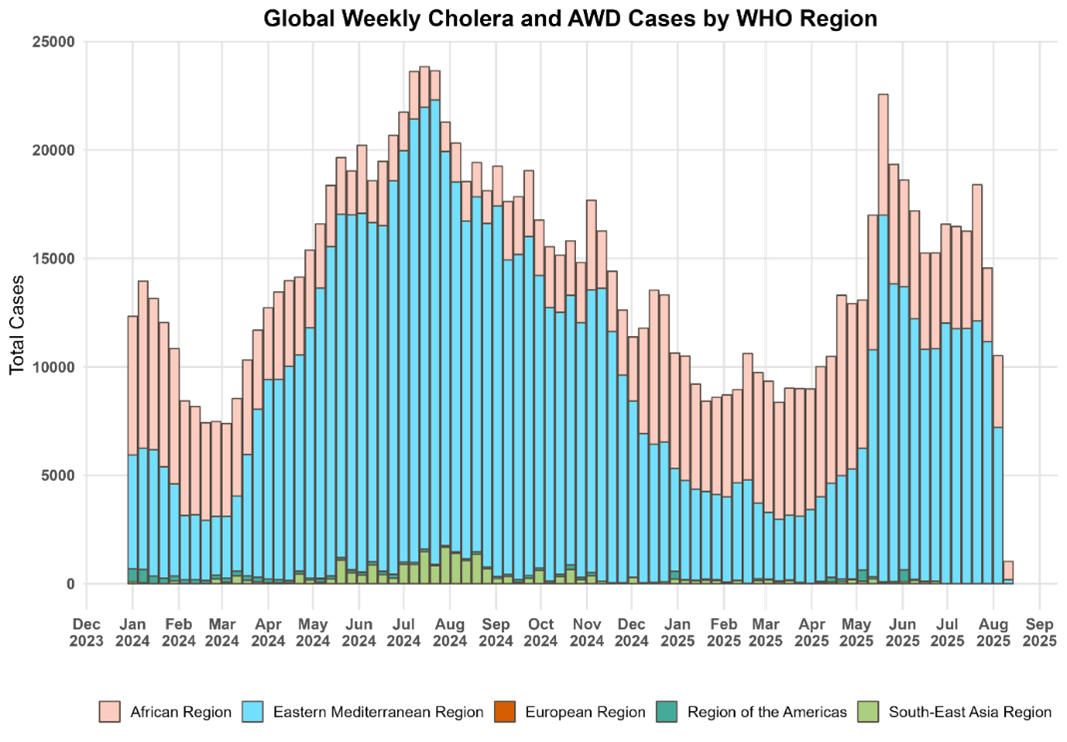
Figure 3. Cholera cases by epidemiological week of reporting (Chad, Republic of the Congo, DRC, South Sudan and Sudan) available as of 17 August 2025. Data source: WHO
Overview of selected countries
Cholera is resurging in a number of countries, including some that have not reported cases in years; the countries highlighted in this report continue to report high transmission rates, case fatality rates, and experience significant challenges in outbreak control and access to care. For a more detailed overview of cholera globally, please refer to the regularly produced global cholera situation report.
Chad
On 24 July 2025, Chad officially confirmed a cholera outbreak, following the report of the first suspected case on 13 July from Dougui Camp in Chokoyane health district, located in Ouaddaï province along the border with Sudan.
Between 13 July and 19 August, the country reported a total of 776 cholera cases, including 53 deaths, resulting in a case fatality rate (CFR) of 6.8%. Of these deaths, 27 occurred in the community, highlighting gaps in timely access to care. Laboratory confirmation has been obtained for 32 cases through culture testing.
As of 19 August, suspected cholera cases have been reported from two provinces (Ouaddaï and Sila) and six health districts: Abdi, Adré, Amleyouna, Chokoyane, Farchana and Hadjer Hadid. Among these, Chokoyane is the most affected, accounting for 541 cases and 25 deaths, with a district-specific CFR of 4.6%.
Republic of the Congo
Between 23 June and 17 August 2025, the Republic of the Congo reported a total of 457 suspected cholera cases and 35 deaths, resulting in a CFR of 7.7 %. The outbreak, which began in the Brazzaville district, has been spreading to districts along the Congo River. Brazzaville has recorded a CFR of 4.8 % (269 cases; 13 deaths), while Congo-Oubangui has experienced a significantly higher CFR of 11.7 % (188 cases; 22 deaths). The most affected age group is 15 to 24 years, accounting for 19% of all reported cases.
Democratic Republic of the Congo
From 1 January to 10 August 2025, the Democratic Republic of the Congo has reported a total of 46 800 cholera cases and 1362 deaths, resulting in a CFR of 2.9%. Cholera cases have been reported in 16 out of the country’s 26 provinces, with Kwango being the most recently affected as of week 31.
During week 32, the country recorded 1887 new cases and 84 deaths, representing a 4.8% and 1.2 % decrease compared to the previous week, respectively. In the past four weeks, 57.4% of all cases have been concentrated in Kinshasa, North-Kivu, South-Kivu and Tshopo provinces. Kinshasa alone has reported 1781 cases and 136 deaths, with a notably high CFR of 8%. In week 31, Kinshasa recorded 126 cases and five deaths, with a weekly CFR of 4%. This shows a declining trend compared with the previous weeks.
South Sudan
From 1 January to 17 August 2025, South Sudan has reported a total of 71 825 suspected cholera cases and 1194 deaths, resulting in a CFR of 1.7 %. The outbreak has affected 55 of 80 counties across eight states and three administrative areas, demonstrating widespread transmission throughout the country. During the most recent reporting month, from 21 July to 17 August 2025, 2472 cases and 36 deaths were recorded nationwide. Between 14 July to 13 August 2025, approximately 74% of the cases reported were concentrated in Unity State, the Abyei Administrative Area, and Central Equatoria. Unity State reported 1562 cases and 10 deaths, Abyei recorded 988 cases and two deaths, while Central Equatoria registered 244 cases and two deaths.
Sudan
Between 1 January and 11 August 2025, Sudan has reported a total of 48 768 cholera and acute watery diarrhoea cases, along with 1094 deaths, resulting in a CFR of 2.2 %. The outbreak has affected all 18 states, with the majority of cases, 72 % reported from Khartoum (22 225 cases), North Kordofan (7394 cases), and White Nile (5622 cases).
Cholera has also been confirmed in all five Darfur states, where both cases and deaths are rising. New areas, including border localities near Chad, have recently reported cases, indicating expanding transmission.
The reported cholera burden varies significantly across the Darfur states. In the northern state, 3687 cases and 26 deaths have been reported, with a CFR of 0.7 %. The southern state has recorded 1589 cases and 66 deaths, resulting in a higher CFR of 4.2 %. The central state has reported 682 cases and nine deaths (CFR 1.3 %), while the eastern state has seen 517 cases and 26 deaths, with a notably high CFR of 5%. The western state has reported 17 cases with no associated deaths.
There are identified gaps in the surveillance system in Darfur, which may lead to delayed reporting from some areas and no reports in others.
Epidemiology
Cholera is an acute diarrheal infection caused by consuming food or water contaminated with the bacterium Vibrio cholerae. It is primarily associated with poor sanitation and limited access to safe water. The disease can cause severe acute watery diarrhoea, resulting in significant morbidity and mortality. The speed of spread depends on exposure levels, population vulnerability, and environmental conditions. Cholera affects both children and adults and can be fatal if left untreated. However, cholera is easily treatable, with most cases successfully managed through prompt administration of Oral Rehydration Solution (ORS).
The incubation period ranges from 12 hours to five days after consuming contaminated food or water. While most infected individuals remain asymptomatic, they can still shed the bacteria in faeces for up to 10 days, potentially spreading the infection to others. Among symptomatic cases, most experience mild to moderate illness, while a smaller proportion develop severe diarrhoea and vomiting, which can lead to life-threatening dehydration.
Humanitarian crises and disasters from natural hazards, such as floods, heighten the risk of cholera transmission by disrupting water and sanitation systems and forcing populations into overcrowded, unsanitary conditions. Controlling cholera outbreaks requires a multisectoral approach, combining surveillance, WASH interventions, adequate case management, social mobilization, community engagement and risk communication and oral cholera vaccination.
Public health response
WHO collaborates closely with Ministries of Health and partners to coordinate cholera response efforts, strengthen surveillance systems, and support diagnostics, case management, and vaccination campaigns. This includes deploying rapid response teams, providing training and supplies for clinical and laboratory staff, supporting WASH and IPC measures in health facilities, and facilitating access to Oral Cholera Vaccines (OCV) through the International Coordinating Group (ICG) mechanism. WHO and partners also promote integrated risk communication and community engagement to support cholera-affected countries through information sharing, training, and development of integrated RCCE plans and tools. In addition, WHO encourages countries to use the Global Task Force on Cholera Control (GTFCC) tools to improve surveillance and guide targeted interventions.
On 26 August, the Africa CDC and WHO launched the Continental Cholera Emergency Preparedness and Response Plan for Africa 1.0, alongside a joint Incident Management Team. This initiative follows the commitment of African Heads of State and Government, who have elevated cholera to a continental priority through their recent high-level Call to Action, pledging to control and eliminate outbreaks by 2030.
Overview of public health response in selected countries
Chad
- Coordination: WHO is working closely with the Ministry of Health and international partners to coordinate response efforts. Cross-border collaboration with Sudan is being supported to address shared challenges.
- Epidemiological Surveillance and Laboratory:
- Daily surveillance updates and sharing of epidemiological situation with all partners.
- Active case finding in Dougi and Hadjer Hadid camps.
- Donation of rapid diagnostic tests (RDTs) and reinforcement of the laboratory for culture confirmation of V. cholerae to reduce the need to transport samples to N’Djamena.
- Case Management: Patient care and prevention efforts continue in affected districts, with hospitalization, isolation, and set-up of initial five cholera treatment centres in Ouddai.
- Supplies: Prepositioning of cholera kits for preparedness in yet to be affected districts, donation of treatment materials (peripheral, central and community kits) to affected districts.
- Infection Prevention and Control /Water, Hygiene, and Sanitation: Critical gaps remain, particularly in areas where water access is below emergency standards and WASH funding is limited. Partners are urged to prioritize WASH in future funding proposals to address waterborne disease risks effectively.
- Risk Communication and Community Engagement: Awareness campaigns are ongoing to promote hand hygiene, latrine use, early care seeking and food safety. RCCE partners are supporting integrated communication strategies.
- Vaccination: The ICG approved a request from the Government of Chad for 870 000 doses for eastern Chad. An additional 250 000 doses were approved as prepositioning stock. Doses will arrive in the country on 29 August, and the campaign will be implemented shortly afterwards.
- Preparedness and Readiness: Anticipating potential spread of the disease, the country is working with partners on preparedness in areas not yet affected. WHO prepositioned cholera kits in at-risk districts.
Democratic Republic of the Congo:
- Coordination: WHO has deployed multidisciplinary teams to Kinshasa to support technical response and coordination. A cross-border coordination meeting with the Republic of the Congo was held on 29 July, with another meeting in planning.
- Epidemiological Surveillance and Laboratory: Technical support provided for cleaning and analysing surveillance data. Training sessions held on the use of cholera rapid diagnostic tests in selected health zones.
- Case Management: Evaluations conducted in cholera treatment centres; medicines and supplies distributed to affected provinces. Hundreds of health technicians and community health workers were trained to support cholera response, including pre-referral care and household distribution of ORS and Aquatabs.
- Infection Prevention and Control /Water, Hygiene, and Sanitation: WASH efforts are ongoing, with WHO providing logistical support and coordination to improve hygiene infrastructure and water quality in affected areas.
- Risk Communication and Community Engagement: Mapping of vulnerable population and mass outreach activities reached over three million people across multiple provinces. Alerts received via call centre and interactive media broadcasts were conducted to promote cholera prevention. Briefings held for community teams and civil society members on communication, infodemic management, and cholera response strategies.
- Vaccination: Since the beginning of the year, three vaccination campaigns have been implemented and targeted 8.6 million people living in 23 health districts of seven provinces. The most recent campaign started on 19 August and targeted 3.7 million people in the city of Kinshasa. A fourth request was approved by ICG to target an additional 2.2 million people in three Provinces of the country. The vaccines are planned to arrive in several lots between 22 and 29 August.
Republic of the Congo
- Coordination: WHO has deployed 33 experts, including epidemiologists, case management experts, RCCE and logisticians. Cross-border coordination with DRC is active.
- Epidemiological Surveillance and Laboratory: Training of 80 community volunteers in Mossaka and Mbamou and provision of 200 cholera RDTs and Yoro and Brazzaville ports. Delivery of 9.5 tonnes of medicines and cholera kits.
- Case Management: Briefing of 172 health workers on case management and IPC, installation of three treatment tents and construction of cholera treatment centres in Mbamou and Mossaka.
- Infection Prevention and Control /Water, Hygiene, and Sanitation: Training on standard precautions and biomedical waste management. Retraining of 22 health workers on standard precautions and chlorination of water at Mossaka base hospital. Establishment of a water supply circuit in Lissanga treatment unit.
- Risk Communication and Community Engagement: Awareness raising conducted for 6023 people, including 318 households. Provision of support to community and religious leaders and distribution of 3000 posters to the Ministry of Health
- Vaccination: An OCV request targeting five health zones was approved by ICG members.
South Sudan
- Coordination: WHO is coordinating with the Ministry of Health (MoH) and partners to manage the outbreak.
- Epidemiological Surveillance and Laboratory:
- WHO is supporting the MoH on routine analysis of reported cases to understand drivers of the outbreak and provision of feedback to the states and counties
- WHO supported the government on the cholera testing algorithm, where sample collection and weekly testing from confirmed locations (3-5 samples) happen.
- Case Management: WHO oversees the ongoing mapping of functional Oral Rehydration Points (ORPs), Cholera Treatment Centers (CTCs) and Cholera Treatment Units (CTUs), within the country. In addition, supported training of health-care providers on case management and community-based volunteers on community case management, provision of supplies to cholera treatment facilities, supported the set-up of oral rehydration points and improvements of cholera treatment facilities.
- Infection Prevention and Control /Water, Hygiene, and Sanitation: WASH interventions are being implemented with WHO support, focusing on hygiene promotion, safe water access, and sanitation improvements.
- Vaccination: Since the beginning of this outbreak, over 10 million OCV doses have been approved and delivered; campaigns have been completed across multiple regions with high uptake in several counties. Post-campaign evaluations are underway.
Sudan
- Coordination: WHO and partners are exploring ways to support cholera response efforts in Sudan and Chad, through technical assistance and potential deployments.
- Infection Prevention and Control/Water, Hygiene, and Sanitation: WASH interventions are being implemented with WHO support, focusing on hygiene promotion, safe water access, and sanitation improvements.
- Vaccination: Since the beginning of the outbreak, 17 requests have been approved through the ICG mechanisms, targeting 25 million people.
WHO risk assessment
As of 17 August 2025, cholera outbreaks continue to escalate across multiple countries, with seven of the 31 countries now reporting case fatality rates above 1%, indicating serious gaps in case management and delayed access to care. Among these, four countries—Chad, the Democratic Republic of the Congo (DRC), South Sudan, and Sudan—are currently classified as being in a major outbreak due to the severity and scale of their outbreaks.
All countries highlighted in this report are facing multiple and similar challenges to control the ongoing outbreaks, underscoring the urgent need for public health interventions and international support.
Cholera outbreaks have been recurrent in several areas of the Democratic Republic of the Congo and South Sudan over the past years. In contrast, Chad and the Republic of the Congo have not reported large-scale outbreaks in recent years. This limited exposure has contributed to low levels of awareness regarding cholera prevention and treatment among both communities and health-care providers, which can contribute to late detection of cases and late care seeking.
Access to affected populations continues to be severely constrained by challenging geography, including outbreaks occurring in remote and hard-to-reach areas such as the Democratic Republic of the Congo and the Republic of the Congo. In Chad, South Sudan, and Sudan, access is further impeded by seasonal flooding and poor road infrastructure, limiting the mobility of both national and international health workers and the timely delivery of essential medical supplies.
These geographic and infrastructural barriers are also hindering the implementation of community programmes, including the decentralization of treatment services. As a result, delays in accessing care are contributing to elevated case fatality rates. The Republic of the Congo and Chad are currently reporting the highest CFRs at 7.7% and 6.8%, respectively. Nearly 50% of reported deaths occur within communities before patients reach health facilities.
Insecurity, population displacement, and the ongoing refugee crisis—particularly in Chad, South Sudan, and Sudan—are compounding these challenges. In these settings, CFRs consistently exceed the 1% threshold, underscoring the impact of restricted access to care. In conflict-affected areas, including parts of Sudan and eastern DRC, insecurity and displacement continue to obstruct surveillance activities and limit the ability to accurately assess the scope of the outbreaks.
Cross-border population movement, particularly in areas with porous borders and high mobility, further exacerbates the risk of regional spread. Many of these countries share borders and experience frequent migration due to trade, displacement, and conflict, increasing the likelihood of cholera transmission across national boundaries.
Inadequate access to clean water and sanitation remains a common denominator across all affected countries, leaving communities highly vulnerable to cholera outbreaks. Seasonal factors such as heavy rains and flooding further amplify this risk by contaminating water sources and facilitating rapid transmission.
These systemic barriers, coupled with overstretched response capacities, are contributing to high case fatality. There is an urgent need to decentralize treatment services, strengthen surveillance systems, and improve access to lifesaving care to reduce preventable deaths and mitigate the impact of ongoing outbreaks.
Given the scale, severity, and interconnected nature of these outbreaks, the risk of further spread within and between countries is considered very high. Without urgent and coordinated public health measures, including improved case management, WASH interventions, vaccination campaigns, and cross-border collaboration, cholera transmission is likely to expand across countries.
WHO advice
Leadership and coordination
Response to cholera outbreaks requires strong multi-sectoral, multi-partner coordination, ensuring epidemiological data is available to guide coordinated responses across case detection, RCCE, WASH, case management, OCV administration and prevention of further spread. Coordination mechanisms should build on existing mechanisms where available and should be implemented at both national and sub-national levels.
Epidemiological Surveillance and Laboratory
WHO supports the national surveillance systems with the deployment of rapid response teams and assistance for data reporting and analysis. WHO supports diagnostics through the provision of rapid diagnostic test kits, training of clinical staff on sample collection and the use of RDTs, training of laboratory diagnosticians, the development and dissemination of recommendations and tools and provision of materials for laboratory diagnostics.
To strengthen early detection of cases and the monitoring of cholera outbreaks, WHO recommends:
- Deployment of rapid response teams
- Integrate health facility-based surveillance, community-based surveillance and event-based surveillance while also integrating epidemiological data with test results
- Regularly evaluate surveillance systems and use results to strengthen
- Use standard recommended definitions of suspected cholera cases and of acute watery diarrhoea
- Use of rapid diagnostic tests for the early detection of suspected or probable cholera outbreaks
- Systematically record standard case-based data on suspected cholera cases detected by health-facility-based surveillance
- Perform routine analysis of key morbidity and mortality indicators (CFR -health facility-deaths and community deaths) at administrative or health zone levels to orient response activities to target the most affected populations.
- Strengthening laboratory capacity to confirm cholera outbreaks and monitor antimicrobial resistance
- Data sharing and joint intervention planning between neighbouring countries, especially in regions with high cross-border movement, is important to prevent further geographic spread and control importation of cases and or existing outbreaks.
Case Management
In order to improve cholera case management, it is advised to use treatment protocols and clinical materials, and to ensure staff at CTCs, CTUs, and ORPs receive proper training and supervision.
Multiple countries are reporting high CFR and a high proportion of deaths occurring in communities. To reduce cholera deaths, WHO recommends:
- Working with RCCE colleagues to promote awareness of cholera, including the importance of early initiation of ORS and rapidly seeking treatment if symptoms occur
- Ensuring early access to treatment through implementation of community-based treatment strategies, including oral rehydration points and distribution of ORS via Community Health Workers
- Reinforce or set up referral mechanisms, including transport from the community and outpatient community structures to inpatient facilities
- Setting up dedicated cholera treatment structures – these may be integrated into existing health-care facilities or be set up as independent structures
- Training staff to recognize and treat patients with suspected cholera
- Ensure adequate supplies for patient treatment
Infection Prevention and Control (IPC)/Water, Hygiene, and Sanitation (WASH)
WHO recommends strengthening WASH and IPC measures in health-care facilities through regular evaluations, staff training, provision of essential supplies, and proper implementation of protocols to reduce transmission. Priority WASH and IPC activities include:
- Improving WASH in healthcare facilities - adequate quantity and quality of water, availability of toilets
- Ensuring at least minimum infection prevention and control measures are implemented in health-care facilities, and especially cholera treatment facilities
- Provision of safe drinking water
- Water quality monitoring
- Safe excreta disposal
- Distribution of WASH kits in affected communities
- Promotion of protective hygiene practices
Risk Communication and Community Engagement
Risk communication and Community Engagement colleagues work across all response pillars, supporting information exchange between affected populations and public health responders. WHO recommends:
- Community promotion of early care seeking,
- Promotion of preventive hygiene measures – hand and food hygiene
- Supporting implementation and OCV campaigns
- Developing social listening to understand the concerns and any misinformation circulating in affected communities so they can be addressed
- Engagement of communities on the protection of water sources
Vaccination
Oral Cholera Vaccine campaigns are an important tool to control cholera outbreaks when used alongside improvements in water and sanitation. OCV protects affected communities and reduces the impact of the outbreak when timely implemented and reduces the risk and extent of outbreak spread. Single-dose strategies for reactive vaccination are currently in effect. Preventive vaccination campaigns have been suspended since late 2022, and the vaccine shortfall has now stalled reactive vaccination efforts as well. WHO recommends:
- Fostering the preparedness and the definition of vaccination strategies for outbreak response
- Submission of a timely and targeted ICG request for reactive vaccination campaign
- Strong risk communication to inform communities about campaigns, enhance demand, maximise uptake and build trust around vaccine safety and efficacy
- Integration of RRCE into vaccination plans
- Readiness and timely implementation of vaccination campaigns
- Fostering sound evaluation and impact assessment of reactive vaccination campaigns
WHO does not recommend travel or trade restrictions to and from the cholera outbreak-affected countries.
Further information
- WHO Cholera factsheet
- Ending Cholera, A Global Roadmap to 2030
- WHO. Water, sanitation and hygiene and infection prevention and control measures for infectious diarrhoea in health-care settings
- GTFCC fixed ORP interim guidance and planning
- Public health surveillance for cholera, Guidance document, 2024
- Recommendations for reporting cholera to the regional and global levels, 2025
- AFRO Weekly outbreaks and emergency bulletin
- Guidelines & technical documents – GTFCC
- WHO AFRO Cholera Dashboard
- Cholera upsurge (2021-present) web page
- GTFCC OCV Dashboard
- Cholera continental preparedness and response plan for Africa
- Multi-country outbreak of cholera, external situation report #29 -28 August 2025
[1] Please note that the data presented here should be interpreted with caution due to potential reporting delays. Such delays may affect the timeliness of reports, and consequently, the presented figures might not accurately represent the current situation.
Citable reference: World Health Organization (29 August 2025). Disease Outbreak News; Cholera-Multi-country with a focus on countries experiencing current surges. Available at: http://www.who.int/emergencies/disease-outbreak-news/item/2025-DON579
