
5.1 Universal Health Coverage and TB
Universal health coverage (UHC) means that everyone can obtain the health services they need without suffering financial hardship (1). Target 3.8 of the United Nations (UN) Sustainable Development Goals (SDGs) is to achieve UHC by 2030 (2). The milestones and targets for reductions in TB incidence and TB mortality set in the World Health Organization (WHO) End TB Strategy can only be achieved if everyone who develops TB disease can access high-quality treatment.
The SDGs include two UHC indicators: (i) the service coverage index (SCI); and (ii) the proportion of the population with large household expenditures on health as a share of total household income or expenditure.
Estimates of the SCI at global, regional and country levels are currently available for 2000–2021 (1,3). Estimates for 2000–2023 are in development and scheduled for publication in December 2025. In the interim, this webpage reproduces the content included in the Global tuberculosis report 2024 (4).
Worldwide, there were steady improvements in the SCI between 2000 and 2019, from a score of 45 (out of 100) in 2000 to 68 in 2019 (Fig. 5.1.1a). Most of this progress occurred between 2000 and 2015 and was primarily due to improvements in service coverage for infectious diseases (with only limited changes for other areas of service provision).
At regional level, the SCI increased in all six WHO regions between 2000 and 2019; the biggest gains were in the South-East Asia and Western Pacific regions. There were also increases in all four World Bank income groups (Fig. 5.1.1b).
In 2020 and 2021, during the COVID-19 pandemic, progress stalled globally (at a value of 68 in 2021) and in most WHO regions and World Bank income groups. In 2021, the WHO regions with the highest values were the European Region (81) and the Region of the Americas (80); the African Region had the lowest value (44).
Fig. 5.1.1 Trends in the UHC service coverage index in WHO regions and World Bank income groups, 2000–2021
(a) By WHO regionsa
(b) By World Bank income groups
Source: World Health Data Hub (https://data.who.int/)
Among the 30 high TB burden countries, most made progress between 2000 and 2019 (Fig. 5.1.2). The largest gains in absolute terms (+30 index point or more) were in China, India, Myanmar, Thailand and Viet Nam. During the COVID-19 pandemic, progress stalled or reversed in most countries. In 2021, the countries with the highest SCI values (around 80) were Brazil, China and Thailand; most other countries had values between around 40 and 60.
Fig. 5.1.2 Trends in the UHC service coverage index in the 30 high TB burden countries, 2000–2021
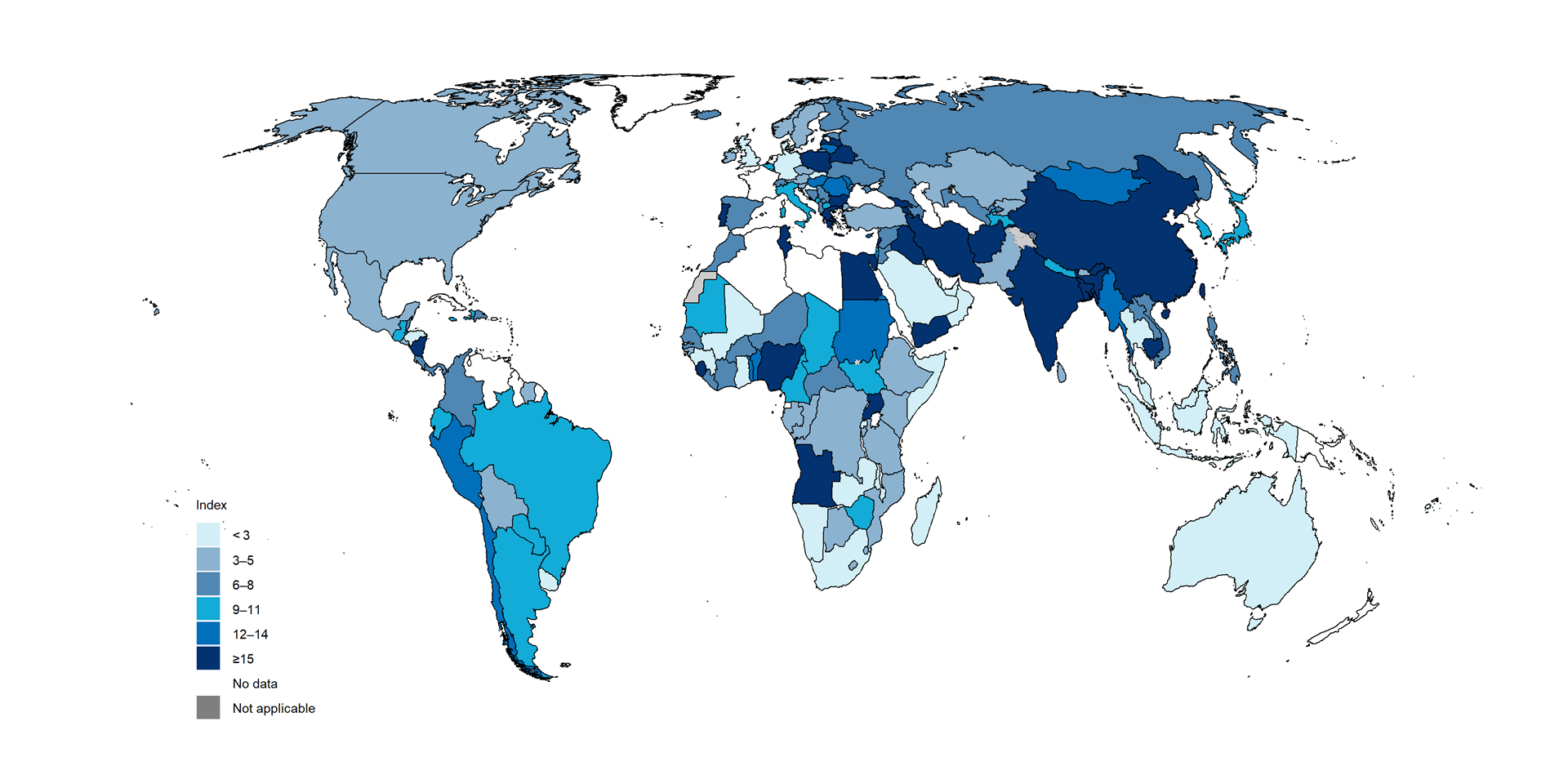
Across all countries, there was a great deal of variation in the SCI in 2021 (Fig. 5.1.3). The highest values were in high-income countries in North America, western Europe and parts of the WHO Western Pacific Region; the lowest values were predominantly in countries in the WHO African Region.
Fig. 5.1.3 UHC service coverage index by country, 2021

In contrast to improvements in the SCI, the global level of financial protection for health expenditures worsened between 2010 and 2019 (estimates for later years are not currently available). Worldwide, the percentage of the general population facing catastrophic expenditure on health (defined for SDG Indicator 3.8.2 in 2017 as >10% annual household income or expenditure) rose from 11.4% (794 million people) in 2010 to 13.5% (1.04 billion people) in 2019 (1, 5). At regional level, higher percentages in 2019 compared with 2010 were estimated for all WHO regions except the Region of the Americas (Fig. 5.1.4) (5).
Fig. 5.1.4 Trends in the percentage of the general population facing catastrophic health expenditurea, globally and for WHO regions, 2000–2019
Source: Global Health Observatory (https://www.who.int/data/gho)
National values are available for different years and there is more geographical variability compared with the SCI, including within regions (Fig. 5.1.5). Of the 30 high TB burden countries, seven had particularly high levels of catastrophic health expenditure (≥15% of the general population): Angola, Bangladesh, China, India, Nigeria, Sierra Leone and Uganda.
Fig. 5.1.5 Percentage of the general population facing catastrophic health expenditurea at country level, latest available year of datab
b The latest available year ranges from 1995 to 2021.
Source: Global Health Observatory (https://www.who.int/data/gho)
The distribution of the two UHC indicators in the 30 high TB burden countries shows that, in general, values improve with income level; this is especially evident for the SCI (Fig. 5.1.6). Nonetheless, as also illustrated in Fig. 5.1.5, the risk of catastrophic health expenditure is high (15% or above) in several middle-income countries, including Angola, Bangladesh, China, India and Nigeria. Thailand stands out as a high TB burden country with both a very high SCI (80 or above) and a high level of financial protection (2% of households facing catastrophic health expenditure). A UHC scheme was established in 2002, supported by domestic funding and a strong primary health care system (6).
Fig. 5.1.6 UHC service coverage index (SDG Indicator 3.8.1)a and percentage of the general population facing catastrophic health expenditure (SDG Indicator 3.8.2),b 30 high TB burden countries,c stratified by World Bank income groupsd
b Defined in 2017 as >10% of total household consumption or income. The latest available year (based on data published in 2023) ranges from 2007 to 2021 for the 30 high TB burden countries.
c Data for SDG indicator 3.8.2 were not available for the Democratic People’s Republic of Korea and Papua New Guinea.
d The classification is for the latest year for which data for SDG Indicator 3.8.2 are available.
Source: Global Health Observatory (https://www.who.int/data/gho)
To achieve UHC, substantial increases in investment in health care are critical. From 2000 to 2022, there were striking increases in health expenditure (from all sources) per capita in a small number of high TB burden countries, notably the upper-middle-income countries of Brazil, China, South Africa and Thailand (Fig. 5.1.7). There have also been considerable increases in several lower-middle-income countries: Bangladesh , India, Indonesia, Kenya, Lesotho, Mongolia, Myanmar, the Philippines and Viet Nam. Health expenditure has been rising in most low-income and high TB burden countries, most noticeably in the Central African Republic, Ethiopia, Liberia and Mozambique, albeit from much lower levels.
Fig. 5.1.7 Current health expenditure per capita, 30 high TB burden countries, 2000–2022, stratified by income groupa
(a) Low-income countries
(b) Lower-middle-income countries
(c) Upper-middle-income countries
Sources: WHO Global Health Expenditure Database ( http://apps.who.int/nha/database/)
References
World Health Organization/World Bank. Tracking Universal Health Coverage: 2023 Global monitoring report. Geneva: World Health Organization; 2023 (https://iris.who.int/handle/10665/374059). License: CC BY-NC-SA 3.0 IGO.
Sustainable development goals: Goal 3 targets and indicators [website]. New York: United Nations (https://sdgs.un.org).
World Health Datahub (https://data.who.int/).
Global tuberculosis report 2024. Geneva: World Health Organization; 2024 (https://iris.who.int/handle/10665/373828). License: CC BY-NC-SA 3.0 IGO.
Global Health Observatory (https://www.who.int/data/gho).
Tangcharoensathien V, Witthayapipopsakul W, Panichkriangkrai W, Patcharanarumol W, Mills A. Health systems development in Thailand: a solid platform for successful implementation of universal health coverage. Lancet. 2018;391(10126):1205–23 (https://pubmed.ncbi.nlm.nih.gov/29397200/).
General disclaimers
The designations employed
and the presentation of the material in this publication do not imply
the expression of any opinion whatsoever on the part of WHO concerning
the legal status of any country, territory, city or area or of its
authorities, or concerning the delimitation of its frontiers or
boundaries. Dotted and dashed lines on maps represent approximate border
lines for which there may not yet be full agreement.
