
5.3 TB determinants
The tuberculosis (TB) epidemic is strongly influenced by broader social and economic development as well as (often interrelated) risk factors more specifically linked to health, such as nutritional status, diabetes, HIV infection, alcohol use disorders and smoking.
For example, the numbers of people developing TB and dying from the disease started to decline in western Europe, North America and some other parts of the world around the turn of the 20th century, as incomes grew, levels of poverty fell, and housing and nutrition improved (1, 2). The fastest declines in TB incidence and TB mortality in western Europe occurred in the 1950s and 1960s, in the context of progress towards universal health coverage (UHC), rapid social and economic development, and the availability of effective drug treatments.
Achieving global targets for reductions in TB disease burden set in the United Nations (UN) Sustainable Development Goals (SDGs) and World Health Organization (WHO) End TB Strategy requires progress in addressing TB determinants. For this reason, WHO developed a framework for monitoring SDG indicators related to TB in 2017; this comprises 14 indicators for which a relationship with TB incidence could be established, under seven SDGs (see Annex 5 of the core report document). Five are health-related risk factors for TB and six are broader socioeconomic determinants; the other three indicators, two for UHC and one related to current health expenditures, are covered in Section 5.1.
There is a particularly clear relationship between TB incidence and two SDG-related indicators: (a) the population prevalence of undernutrition and (b) gross domestic product (GDP) per capita (Fig. 5.3.1).
Fig. 5.3.1 Relationship between two SDG-related indicators and the TB incidence rate
Each dot represents a country or area.
(a) GDP per capitaa

(b) Prevalence of undernutritiona,b
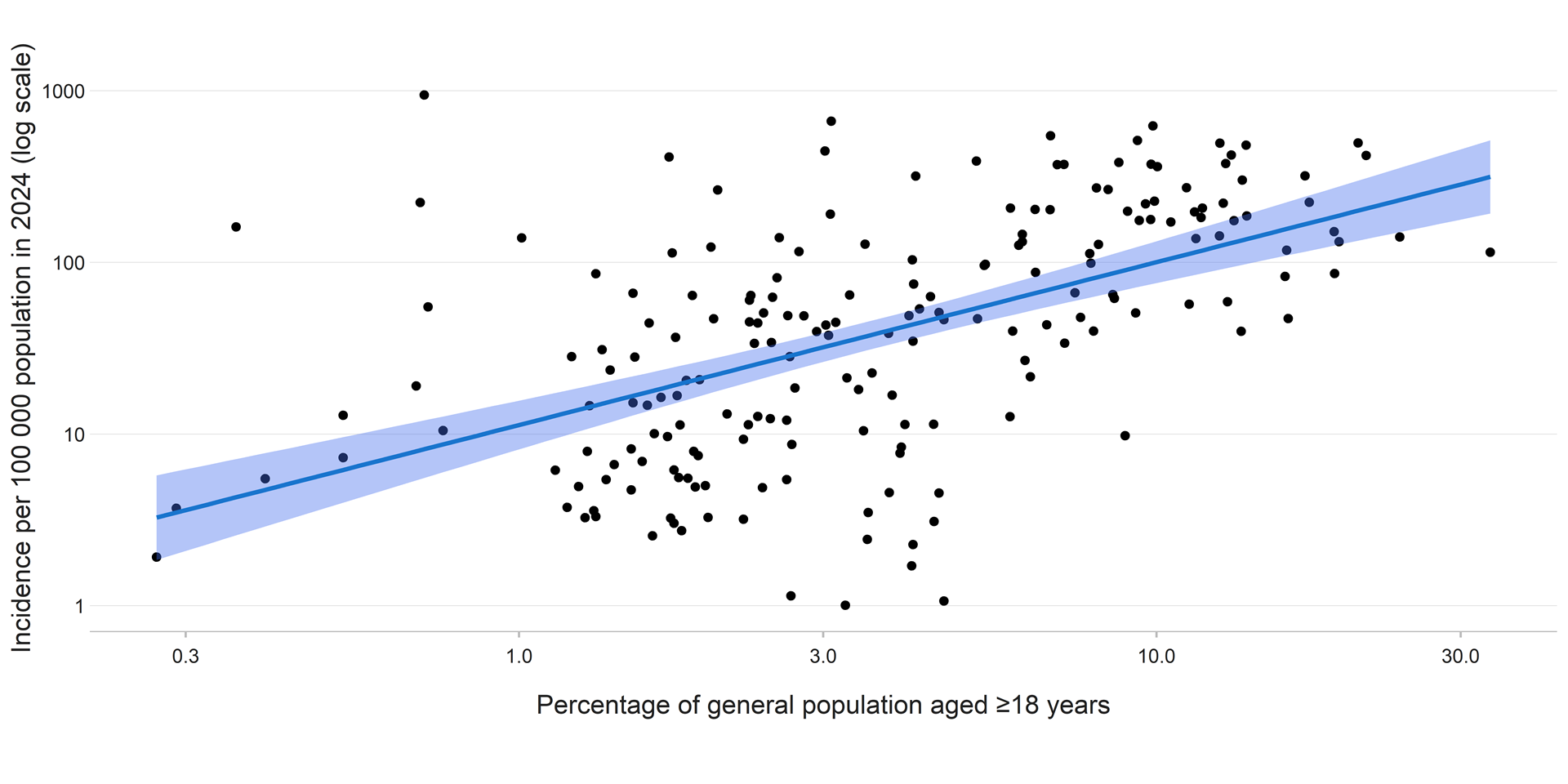
b For adults aged ≥18, undernutrition is defined as a body mass index (BMI) <18.5. For children and adolescents aged 5–17 years, it is defined as a BMI of less than minus 2 standard deviations below the median. For those aged <5 years, it is defined as wasting (weight for height of less than minus 2 standard deviations from the median).
Estimates of the number of people with a new episode of TB (incident cases) attributable to alcohol use disorders, diabetes, HIV infection, smoking and undernutrition are shown in Fig. 5.3.2. Globally in 2024, an estimated 0.97 million incident cases of TB were attributable to undernutrition, 0.93 million to diabetes, 0.74 million to alcohol use disorders, 0.70 million to smoking and 0.57 million to HIV infection (Fig. 5.3.2).
The estimated annual number of cases attributable to diabetes has been revised substantially upwards compared with estimates published in previous WHO global TB reports, following the publication (in 2024) of new estimates of the prevalence of diabetes (for 2022) (3). Previously used estimates of the prevalence of diabetes were for 2014, since when there has been a substantial rise in the global number of people estimated to have diabetes.
Fig. 5.3.2 Global estimates of the number of people with a new episode of TB (incident cases) attributable to five risk factors,a 2024
At country level, there is considerable variation in the relative importance and contribution of the five health-related risk factors (Fig. 5.3.3, Fig. 5.3.4), and thus also variation in which of these factors need to be prioritized as part of national efforts to reduce the burden of TB disease.
Fig. 5.3.3 Estimated population attributable fraction (expressed as a percentage) of people with a new episode of TB (incident cases) attributable to five risk factors,a by country, 2024
(a) Alcohol use disorders

(b) Diabetesb
(c) HIV infection

(d) Smoking

(e) Undernutritionc

b WHO published a systematic review that included an updated estimate of the relative risk of TB associated with diabetes in 2024 (5).
c WHO published a systematic review that included an updated estimate of the relative risk of TB associated with undernutrition in 2024 (7).
Undernutrition, diabetes, alcohol use disorders and smoking are the most important health-related risk factors for TB (in terms of the estimated number of attributable cases) in most of the 30 high TB burden countries (Fig. 5.3.4). Exceptions are Brazil and several countries in the African Region (especially in east and southern Africa), where HIV infection is the leading risk factor.
Fig. 5.3.4 Estimated number of TB cases attributable to five risk factors, 30 high TB burden countries,a 2024
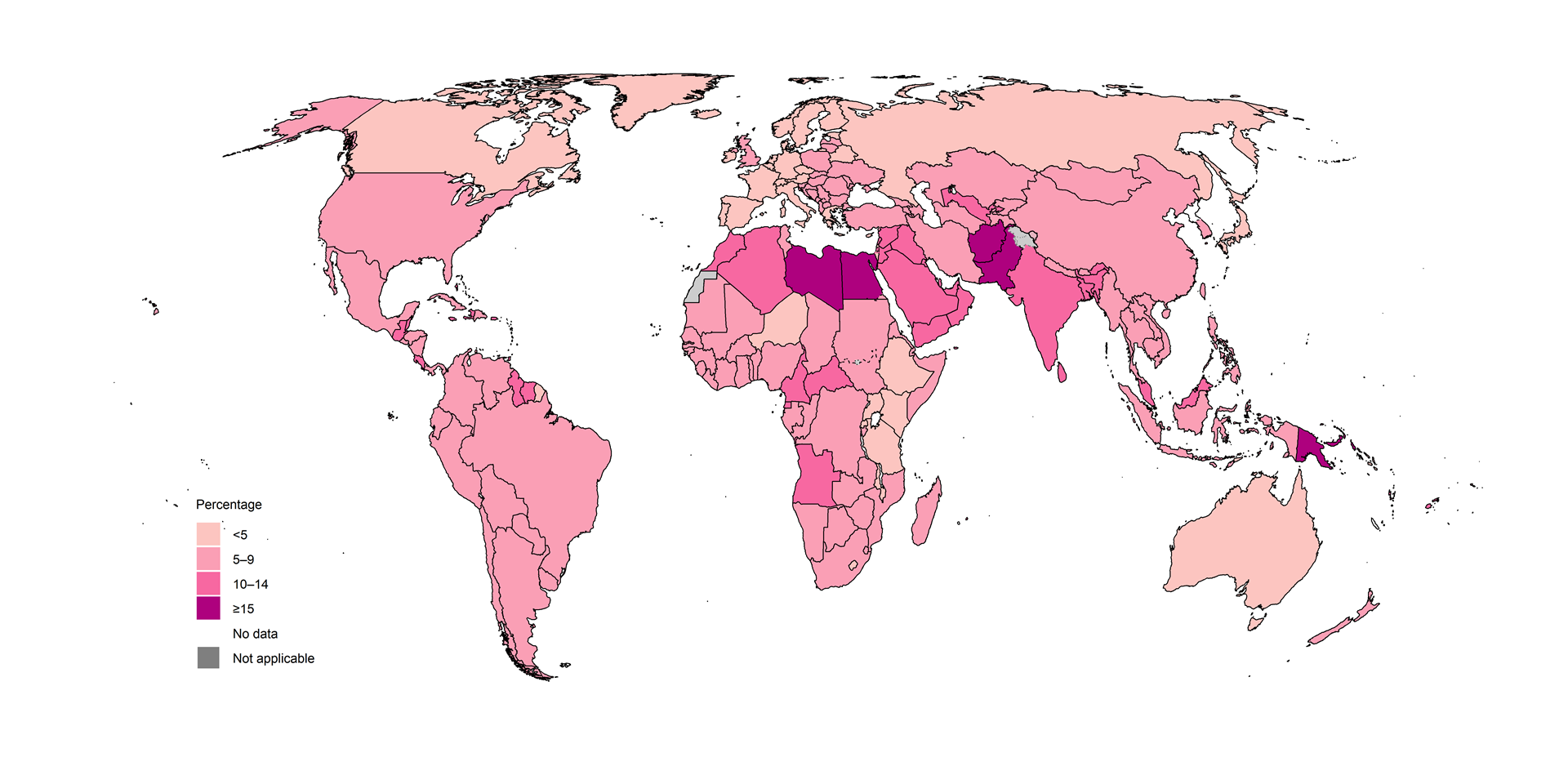
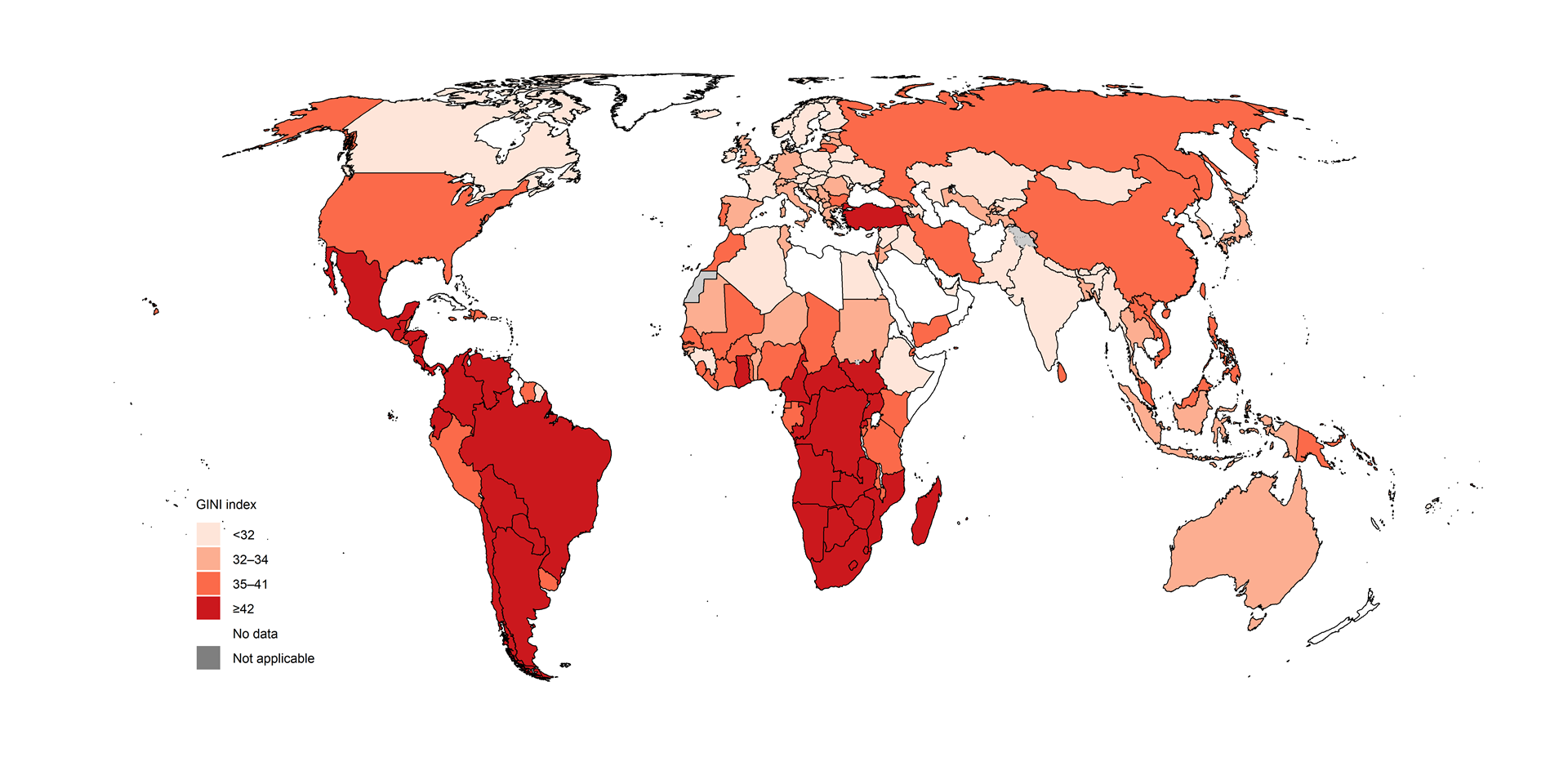
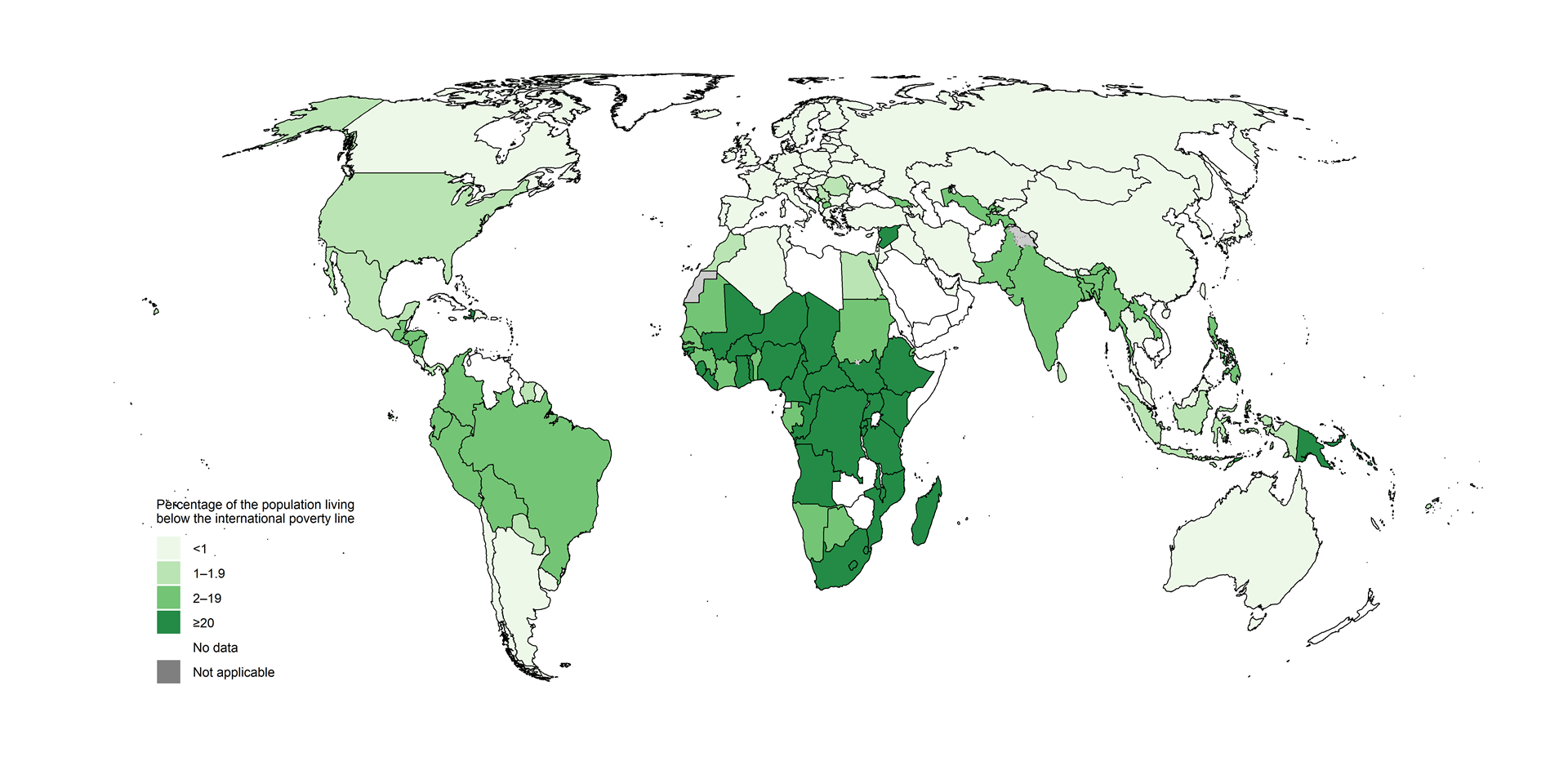
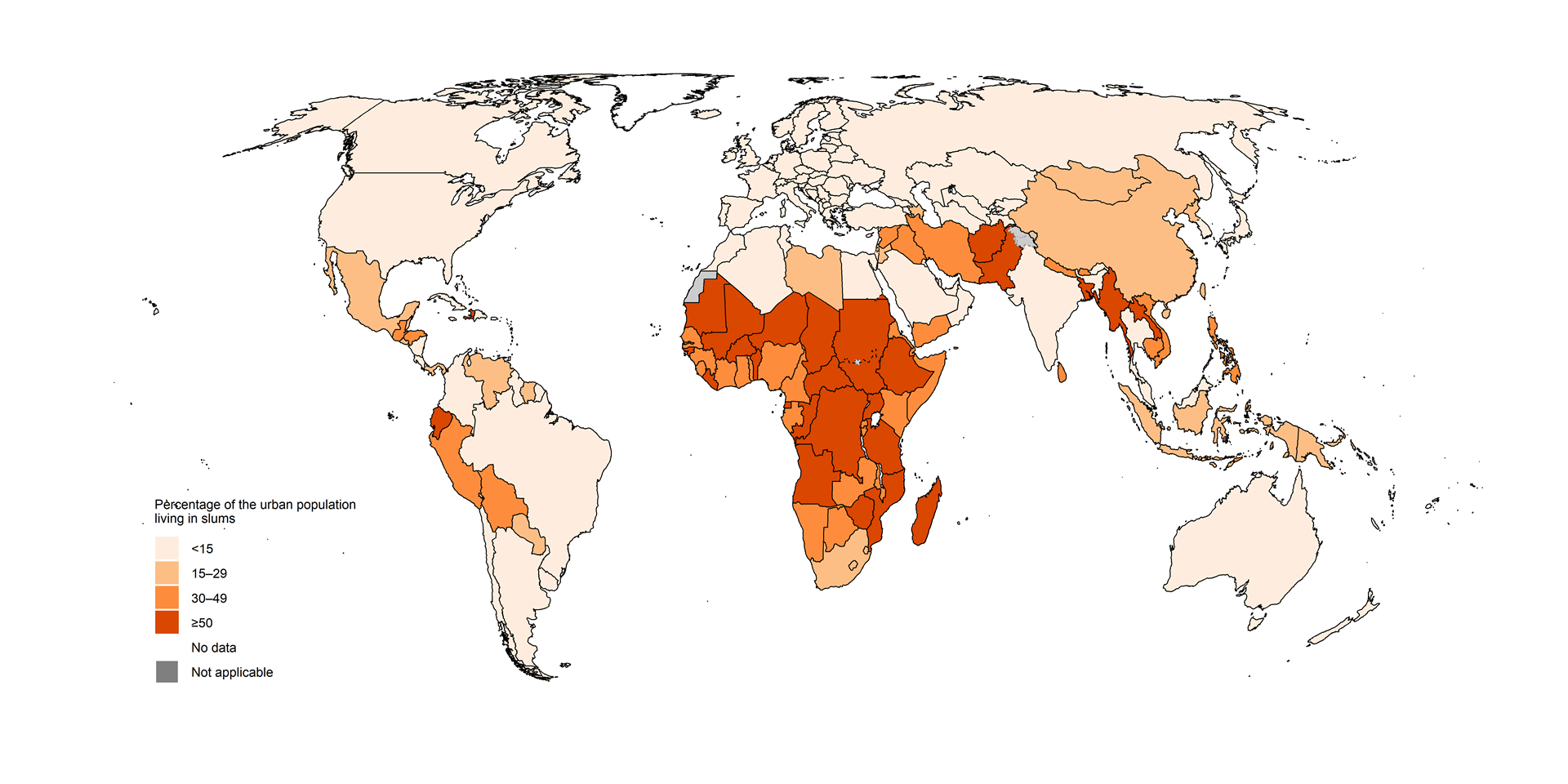
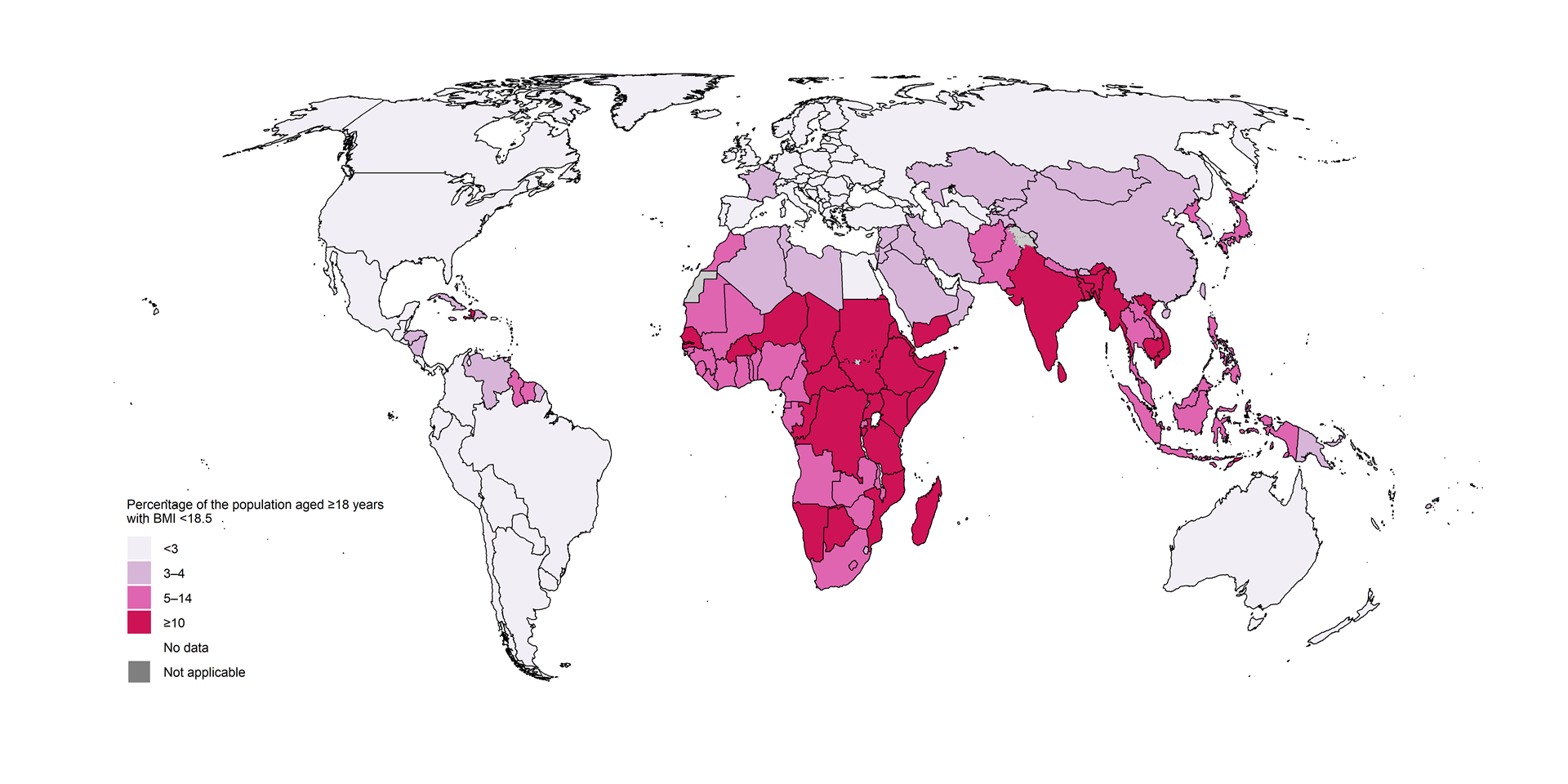
The status of TB determinants beyond those included under SDG 3 is shown in Fig. 5.3.5 Poor access to clean cooking fuels, a high percentage of the population living in poverty, low coverage of social protection and a high percentage of the urban population living in slums are most common in countries in the WHO African Region. The prevalence of undernutrition is comparatively high in countries in the WHO African and South-East Asia regions. Income inequality is highest in countries in the WHO African Region and the Region of the Americas.
Fig. 5.3.5 Status of selected SDG-related indicators beyond SDG 3 at country level, latest available year
(a) Access to clean cooking fuels
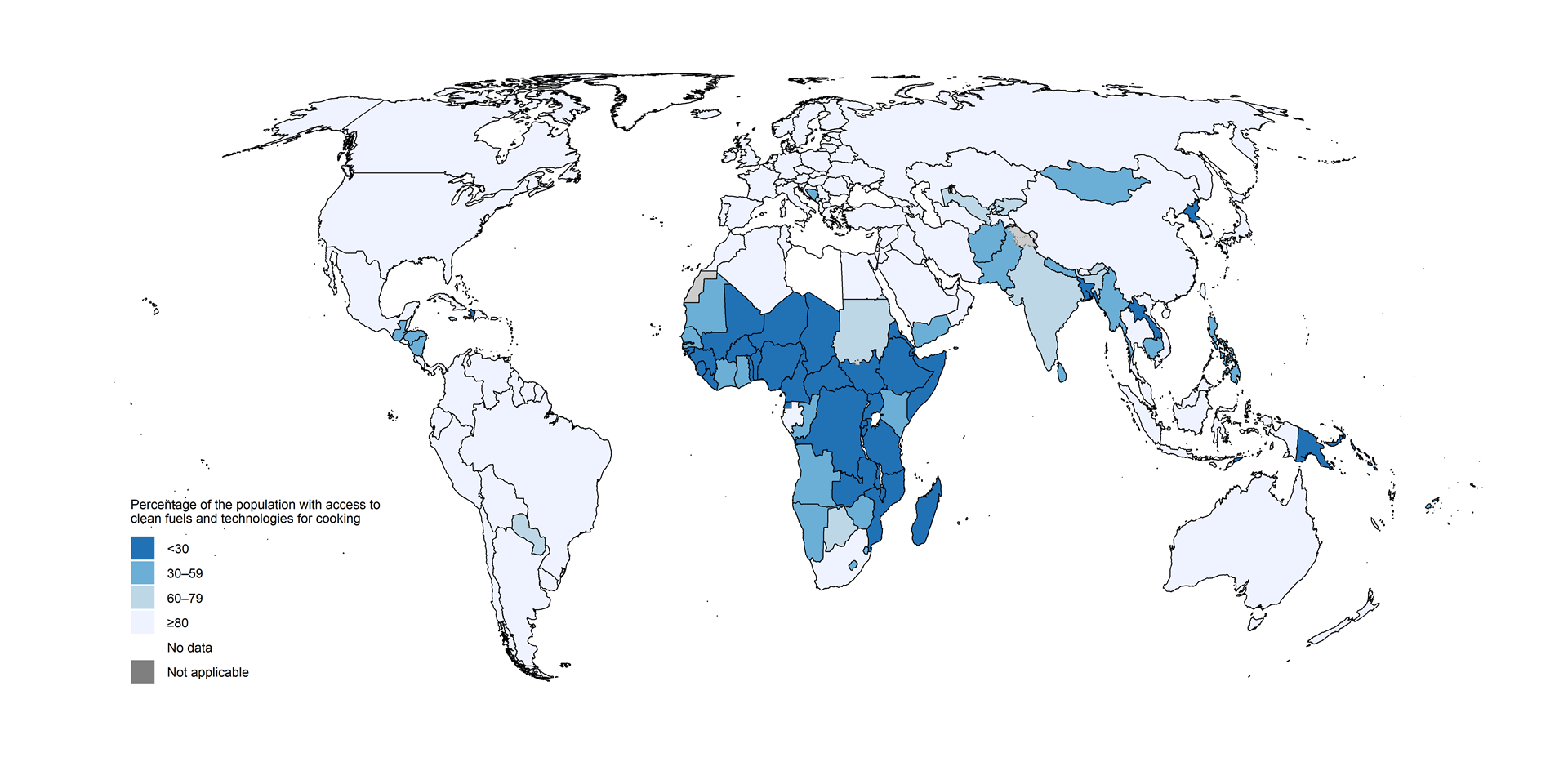
(b) Income inequality
(c) Living in poverty
(d) Access to social protection

(e) Living in slums
(f) Undernutrition
Income inequality: GINI index is shown where 0 is perfect equality and 100 is perfect inequality.
Living in poverty: Percentage of the population living below the international poverty line, which is defined as living on $1.90 per day (at 2017 purchasing power parity).
Access to social protection: Percentage of the population covered by at least one social protection benefit.
Living in slums: Percentage of the urban population living in slums.
Undernutrition: Percentage of the population that is underweight (BMI <18.5), among people aged ≥18 years.
Source: World Bank Sustainable Development Goals Database (http://datatopics.worldbank.org/sdgs/); the WHO Global Health Observatory (https://www.who.int/data/gho)
The most recent data for undernutrition and five socioeconomic indicators associated with TB incidence are shown for the 30 high TB burden countries in Fig. 5.3.6. To facilitate comparisons with two indicators for which the ideal value is 100 (the percentage of the population with access to social protection and the percentage of the population with access to clean fuels), three of the other indicators (the percentage of the urban population living in slums, the percentage of the population with undernutrition and the percentage of the population living below the international poverty line) are represented as their inverse (i.e. the percentage of the urban population not living in slums, the percentage of the population with adequate nutrition and the percentage of the population living above the poverty line). An inverse of the GINI index (a measure of income inequality, which can take values from 0 to 100) is also shown. All indicator values in the figure are for the general population as opposed to people with TB; values for people with TB specifically (e.g. out-of-pocket expenditure and access to social protection) may differ from these general values.
Fig. 5.3.6 Status of selected SDG-related indicators beyond SDG 3 in 30 high TB burden countries, latest available year
Income equality: An inverse GINI index is shown where 0 is perfect income inequality and 100 is perfect income equality.
Not in poverty: Percentage of population living above the international poverty line, which is defined as living on $1.90 per day (at 2017 purchasing power parity).
Social protection: Percentage of the population covered by at least one social protection benefit.
Not in slums: Percentage of urban population not living in slums.
Adequate nutrition: Prevalence of BMI ≥18.5 among people aged ≥18 years.
Source: World Bank Sustainable Development Goals Database (http://datatopics.worldbank.org/sdgs/); the WHO Global Health Observatory (https://www.who.int/data/gho)
Based on the latest available data in the World Bank database, some upper-middle-income and lower-middle-income countries (e.g. Brazil, China, India, Indonesia, Mongolia, South Africa, Thailand and Viet Nam) appear to be performing relatively well in terms of the selected SDG-related indicators. However, values for poor populations and other groups most at risk of developing TB are likely to be worse than national averages. Addressing the broader social and economic determinants of the TB epidemic requires multisectoral action and accountability. Global and national progress in adapting and using the WHO multisectoral accountability framework for TB (MAF-TB) is discussed in Section 5.4.
Further country-specific details for the 14 indicators related to TB incidence are available in the Global tuberculosis report app and Country profiles.
References
Grange JM, Gandy M, Farmer P, Zumla A. Historical declines in tuberculosis: nature, nurture and the biosocial model. Int J Tuberc Lung Dis. 2001;5(3):208–12 (https://www.ncbi.nlm.nih.gov/pubmed/11326817).
Styblo K, Meijer J, Sutherland I. [The transmission of tubercle bacilli: its trend in a human population]. Bull World Health Organ. 1969;41(1):137–78 (https://www.ncbi.nlm.nih.gov/pubmed/5309081).
The Global Health Observatory, 2025, WHO (https://www.who.int/data/gho/data/indicators/indicator-details/GHO/prevalence-of-diabetes-age-standardized)
Imtiaz S, Shield KD, Roerecke M, Samokhvalov AV, Lönnroth K, Rehm J. Alcohol consumption as a risk factor for tuberculosis: meta-analyses and burden of disease. Eur Respir J. 2017;50 (https://pubmed.ncbi.nlm.nih.gov/28705945/).
Franco JVA, Bongaerts B, Metzendorf MI, Risso A, Guo Y, Peña Silva L, Boeckmann M, Schlesinger S, Damen JAAG, Richter B,Baddeley A, Bastard M, Carlqvist A, Garcia-Casal MN, Hemmingsen B, Mavhunga F, Manne-Goehler J, Viney K.Diabetes as a risk factor for tuberculosis disease.Cochrane Database of Systematic Reviews 2024, Issue 8. Art. No.: CD016013. DOI: 10.1002/14651858.CD016013.pub2. (https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD016013.pub2/full)
Lönnroth K, Castro KG, Chakaya JM, Chauhan LS, Floyd K, Glaziou P et al. Tuberculosis control and elimination 2010-50: cure, care, and social development. The Lancet. 2010;375:1814-29 (https://pubmed.ncbi.nlm.nih.gov/20488524/).
Franco JVA, Bongaerts B, Metzendorf MI, Risso A, Guo Y, Pena Silva L et al. Undernutrition as a risk factor for tuberculosis disease. Cochrane Database of Systematic Reviews 2024, Issue 6. Art. No.CD015890. (https://doi.org/10.1002/14651858.CD015890.pub2).
General disclaimers
The designations employed
and the presentation of the material in this publication do not imply
the expression of any opinion whatsoever on the part of WHO concerning
the legal status of any country, territory, city or area or of its
authorities, or concerning the delimitation of its frontiers or
boundaries. Dotted and dashed lines on maps represent approximate border
lines for which there may not yet be full agreement.
