Public financial management
Overview
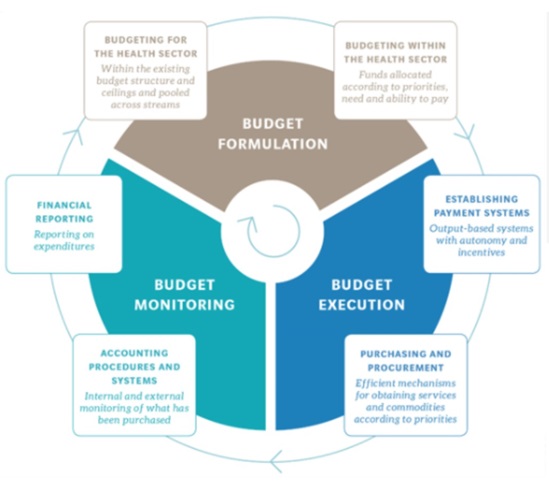
Public financial management (PFM) rules govern how budgets are formed, disbursed and accounted for. This is centrally important to universal health coverage (UHC) to make sure increases in public spending translate into expanded health coverage.
National health authorities should aim to effectively engage with national budgetary authorities to foster credible, priority-oriented health budgets, ensure efficient flows and execution and strengthen accountability.

Why does PFM matter for health finance and UHC?
PFM systems affect health financing in:
- the level and allocation of public funding (budget formulation);
- the effectiveness of spending (budget execution); and
- the flexibility in which funds can be used (pooling, sub-national PFM arrangements and purchasing).
The systems ultimately determine how well health spending can be aligned to meet health coverage and service delivery objectives.
Most of the resources for UHC and the health sector in general will and should come from public budgets. More revenue for the health sector will not help achieve UHC goals if spending cannot be directed to priority populations, programmes and services.
However, countries have limited fiscal resources; growth in public health spending must be in alignment with the macroeconomic and fiscal capacity of the country. Therefore, optimizing how public funds for health are managed and flow through the PFM system is critical for achieving UHC objectives within available resources.
PFM systems and health financing functions must be harmonized to meet objectives to have effective service delivery that can make public funds available for priority populations, programmes and services to meet UHC objectives.
PFM systems and processes (budget formation, budget execution, expenditure control and reporting) must be sufficiently flexible to enable provider payment systems to move from paying for a building with all services provided, to paying for either specific services or for services to specific individuals. Sufficiently flexible PFM is a pre-condition for integrating strategic health purchasing.
A key step to implementation is therefore the ability to target health budget funds to priority services (such as maternal and child health) and specific populations (such as the poorest). This means that clearly defined priorities can be realized (or purchased) in practice.
How to enhance alignment between PFM and health financing ?
As countries plan health financing improvements to address the specific challenges of the health sector, it is important for health policy-makers to understand the PFM system and any ongoing reforms in order to frame and guide dialogue with the ministry of finance. There are specific challenges with alignment of PFM and health financing reform objectives related to each health financing function.
Revenue raising
The health sector requires sufficient and stable resources to meet stated objectives, and funds must be raised equitably and efficiently.
Pooling
Effective pooling of public funds requires both a mandate and a fiscal mechanism to accumulate funds for health based on the ability to pay and reallocate them according to need.
Purchasing
Strategic purchasing requires flexibility to allocate funds to pay for outputs and outcomes, and well-functioning information systems to design, implement and monitor purchasing mechanisms.
Publications
All ->
The ongoing COVID-19 pandemic has shown that public financial management (PFM) should be an integral part of the response. Effectiveness in financing the...
Leveraging public financial management for better health in Africa: key bottlenecks and opportunities...
Why PFM matters for health?Public financial management is at the core of UHC. A robust PFM system is integral to enabling progress towards UHC. Subject...

Robust public budgeting in the health sector is a necessary condition to enable the effective implementation of health financing reforms towards universal...
Public financing for UHC: towards implementation
From 31 October through 2 November 2018, WHO’s Department of Health Systems Governance and Financing convened the third in a series of meetings related...
This report takes stock of the main public financing for health trends over the past fifteen years in the African region, and highlights opportunities...
Events
Self-paced course
News