
4.1 Financing for TB prevention, diagnostic and treatment services
Progress in reducing the burden of tuberculosis (TB) disease requires adequate funding sustained over many years. The World Health Organization (WHO) began annual monitoring of funding for TB prevention, diagnostic and treatment services, based on data reported by national TB programmes (NTPs) in annual rounds of global TB data collection, in 2002. Findings have been published in global TB reports and peer-reviewed publications (1–3). Recognizing that not all international donor funding for TB is captured in the data reported to WHO, each year WHO complements its analysis of data reported by NTPs with an assessment of international donor funding for TB using donor reports to the Organisation for Economic Co-operation and Development (see Section 4.2). Since 2005, funding for TB research has been monitored by Treatment Action Group, with findings published in an annual report (4).
At the second United Nations (UN) high-level meeting on TB in 2023, Member States committed to mobilizing at least US$ 22 billion per year for TB prevention, diagnostic and treatment services by 2027, and US$ 35 billion per year by 2030; a target of US$ 5 billion per year by 2027 was set for investment in TB research (5). These targets were based on estimates of resource needs set out in the latest Global Plan to End TB produced by the Stop TB Partnership (6).
At the outset, it is important to acknowledge that following decisions by the United States government (USG) in early 2025, the landscape of international donor funding in general, including for TB specifically, has changed substantially. Although it is too early for a reliable assessment of funding for the TB response in 2025, this webpage includes a new graphic that shows the share of NTP funding in 2024 that was provided by bilateral grants from the United States Agency for International Development (USAID), grants from the Global Fund and domestic sources. For the 21 countries that reported data (out of a total of 24 that were USAID priorities for bilateral funding for TB in 2024), this provides an indication of the extent to which reductions in international donor funding could impact TB prevention, diagnostic and treatment services in 2025.
A complementary assessment of the impact of funding cuts on TB services in 2025, based on provisional TB case notification data for 2025 that have been reported to WHO as well as information shared with WHO about how NTP activities and TB services have been affected, is one of the “featured topics” of this year’s report. Modelling analyses of the potential effects of USG funding cuts on TB disease burden (symptomatic episodes of TB disease and deaths due to TB) have been published elsewhere (7–10).
Funding available for TB prevention, diagnostic and treatment services
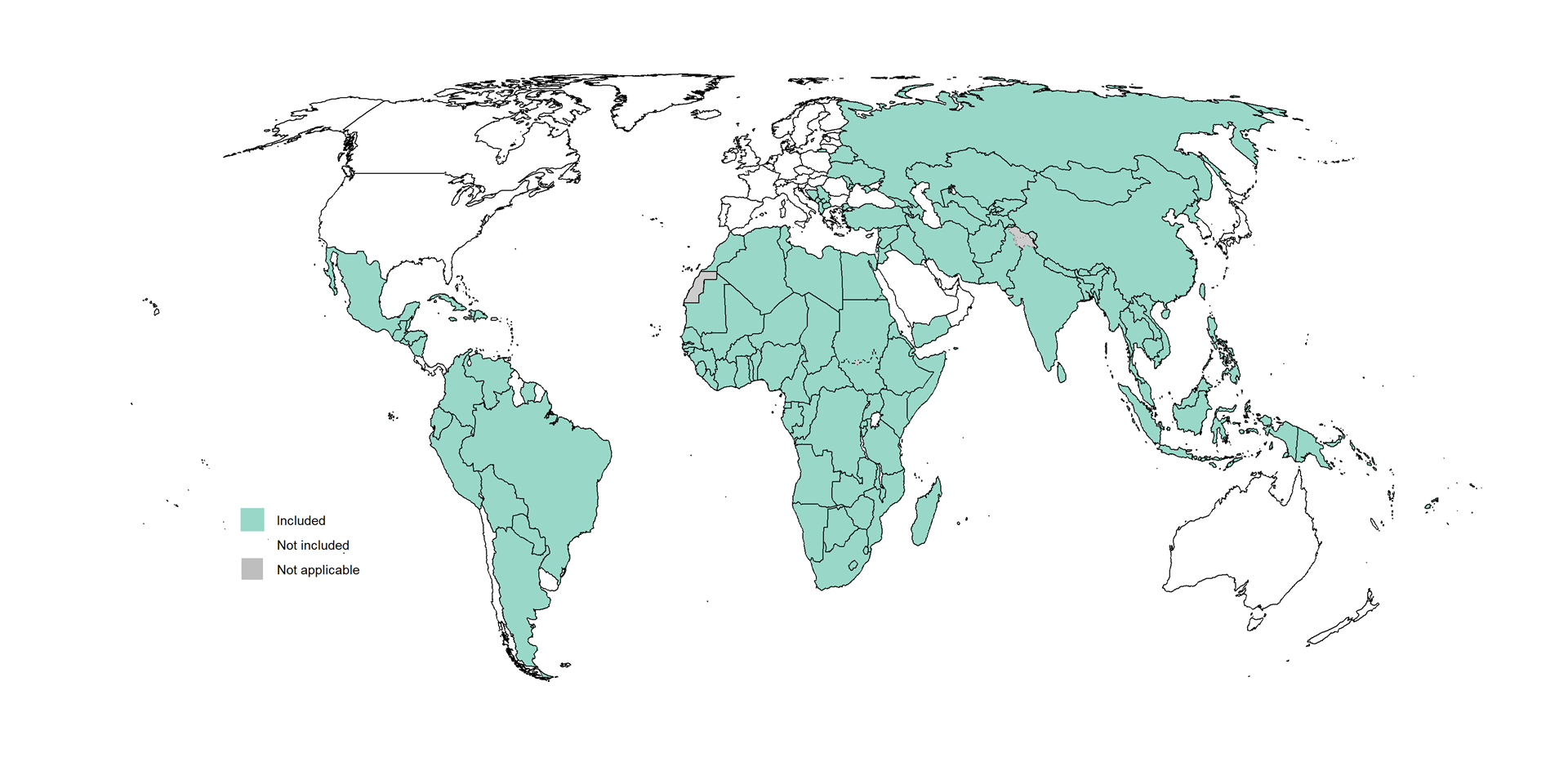
Data about funding available for TB prevention, diagnostic and treatment services by major category of expenditure and source of funding in the 10-year period 2015–2024 have been reported to WHO by 131 low and middle-income countries (LMICs) (Fig. 4.1.1). These countries accounted for 99% of reported TB cases globally in 2024.
Fig. 4.1.1 The 131 low- and middle-income countriesa included in WHO analyses of TB financing, 2015–2024
Funding available for TB prevention, diagnostic and treatment services in LMICs falls far short of the global targets set at the 2023 UN high-level meeting. In 2024, the total funding available in LMICs was US$ 5.9 billion; this was a slight increase from US$ 5.8 billion in 2023, but equivalent to only 27% of the target of reaching US$ 22 billion annually by 2027. The level of funding in LMICs has been relatively stable since 2020, hovering around US$ 6 billion per year (Fig. 4.1.2).
Fig. 4.1.2 Funding available for TB prevention, diagnostic and treatment services in 131 low- and middle-income countries by source,a,b,c,d 2015–2024
b The 131 countries accounted for 99% of the global number of notified cases of TB in 2024. In a small number of countries (nine countries in 2024, which accounted for 0.50% of the number of TB cases notified globally), TB funding data for 2024 were not reported to WHO and funding amounts could not be estimated from available data. For these countries, only the estimated financial costs associated with inpatient and outpatient treatment were included.
c In the most recent classification of countries by income group published by the World Bank (11), the Russian Federation was categorized as a high-income country. It was included in all analyses because it was an upper-middle-income country for most of the period 2015–2024, is in WHO’s list of high burden countries for drug-resistant TB and is one of the three countries in WHO’s list of global TB watchlist countries (having been in WHO’s list of high TB burden countries until 2020). For more details about WHO’s lists of high burden countries for TB, drug-resistant TB and TB/HIV, see Annex 3 of the core report document.
d Domestic funding in this graphic includes data reported by NTPs and the financial costs associated with inpatient and outpatient care required during TB treatment, estimated by WHO. For further details, see Box 4.1.
Throughout the period 2015–2024, funding available by source shows a consistent pattern in terms of the relative contributions from domestic and international donor sources (Fig. 4.1.2). In 2024, 82% of the funding available for TB prevention, diagnostic and treatment services was from domestic sources, similar to previous years. Overall, international donor funding for LMICs has remained stable throughout the period 2015–2024, ranging from around US$ 1.1 to US$ 1.2 billion per year.
Aggregate figures for the shares of funding from domestic and international sources in LMICs are strongly influenced by five countries: Brazil, the Russian Federation, India, China and South Africa (BRICS) (Fig. 4.1.3). In combination, these five countries accounted for US$ 3.1 billion (64%) of the total of US$ 4.8 billion in 2024 that was provided from domestic sources. Overall, 96% of available funding in BRICS and all funding in Brazil, China and the Russian Federation in 2024 was from domestic sources.
In other LMICs, international donor funding remains crucial. For example, in 2024, such funding accounted for 54% of the funding available in the 26 high TB burden and two global TB watchlist countries (Cambodia and Zimbabwe) outside BRICS, and 63% of the funding available in low-income countries (LICs).
Fig. 4.1.3 Funding available for TB prevention, diagnostic and treatment services from domestic sourcesa and international donors in nine country groups, 2015–2024
a Domestic funding in this graphic includes data reported by NTPs and the financial costs associated with inpatient and outpatient care required during TB treatment, estimated by WHO. For further details, see Box 4.1.
b BRICS is used to refer only to the five original members of the BRICS group of countries, acknowledging that this group expanded in 2024 and in 2025 comprises 11 countries.
c The two global TB watchlist countries included are Cambodia and Zimbabwe.
d Asia includes the WHO regions of South-East Asia and the Western Pacific.
e “Other regions” consists of three WHO regions: the Eastern Mediterranean Region, the European Region and the Region of the Americas.
The main source of international donor funding for TB is The Global Fund (13). Its share of the total amount of international donor funding reported by NTPs to WHO was 73% in 2024.
Section 4.2 provides a more comprehensive analysis (for the period of 2013–2023), including additional funding that is not channeled through NTPs. A key finding, especially in the context of USG decisions in early 2025, is that the USG was the largest contributor of funding to The Global Fund and also the largest bilateral donor for TB; overall, it accounted for about 50% of international donor funding for TB in the period of 2013–2023.
For 21 countries that reported data to WHO about the amount of bilateral funds received from USAID in 2024 (out of a total of 24 priority countries that were eligible to receive such funds), the share of these funds as a percentage of the total available funding reported by NTPs in 2024 is shown in Fig. 4.1.4. USAID bilateral funds accounted for 20% or more of the total available funding in 13 of these countries, with the highest share (over 30%) in Zambia and Cambodia. Almost all of the countries that received USAID bilateral funds for TB were also highly reliant on Global Fund grants in 2024 (the main exception was India). In 2025, the Global Fund has anticipated reductions in contributions due to changes in the landscape of funding for global health, and requested countries to pause or defer activities as a first step. As of July 2025, funding for the 2024–2026 grant cycle (for HIV, TB and malaria) had been cut by US$ 1.4 billion, equivalent to 11% of the original allocation (14).
Fig. 4.1.4 Sources of funding availablea for TB prevention, diagnostic and treatment services in 2024, for 21 countriesb that reported receiving Global Fund grants and bilateral funding from USAID in 2024
a Domestic funding in this graphic is based on data reported by NTPs, which typically do not include the financial costs associated with inpatient and outpatient care required during TB treatment.
b There were an additional three countries that were USAID priorities for bilateral funding for TB in 2024 for which data were not available: Pakistan, Uzbekistan and Viet Nam.
Brazil, India, Mongolia, the Philippines and Sierra Leone are
examples of high TB burden countries that have increased domestic
funding specifically allocated to NTPs in recent years
(Fig. 4.1.5). There
were also substantial increases up to 2023 in Bangladesh, up to 2019 in
China and in 2023 in Lesotho. In Cambodia, one of the global TB
watchlist countries, domestic funding rose from 2015–2020 but
subsequently levelled off.
There are also countries where domestic funding reported by NTPs has noticeably decreased in recent years: Kenya, Nigeria and South Africa. In South Africa, this is consistent with a substantial decline in case notifications of people newly diagnosed with TB (see Fig. 2.1.2 of Section 2.1) and in estimated levels of TB incidence (see Fig. 1.1.11 of Section 1.1). In addition, the implementation and scale-up of all-oral 9-month and 6-month regimens for people diagnosed with drug-resistant TB (see Fig. 2.4.10 of Section 2.4) has reduced health service utilization, and associated WHO estimates of domestic funding used for inpatient and outpatient care. In Kenya, the decline in domestic funding available to the NTP has been compensated for by increases in international donor funding. In Nigeria, the average utilization of inpatient and outpatient care during TB treatment has reduced considerably since 2019.
Fig. 4.1.5 Funding available for TB prevention, diagnostic and treatment services in the 30 high TB burden countries and three global TB watchlist countries,a disaggregated by source of funding, 2015–2024
a The three global TB watchlist countries are Cambodia, the Russian Federation and Zimbabwe; for further details, see Annex 3 of the core report document.
The funding available for diagnosis and treatment of drug-susceptible TB fell from 2017–2022, but grew slightly in 2023 and remained stable in 2024 (Fig. 4.1.6). Funding available for treatment and management of drug-resistant TB increased from 2015–2022, but then declined in 2023 and again in 2024. These patterns are largely explained by trends in BRICS (Fig. 4.1.7).
Fig. 4.1.6 Funding available for TB prevention, diagnostic and treatment services in total and by category of expenditure in 131 low- and middle-income countries,a 2015–2024
b The category of drug-susceptible TB includes funding reported by NTPs for the following items: laboratory equipment and supplies; anti-TB drugs; programme management (including staff and activities); operational research and surveys; patient support; and miscellaneous items. It also includes WHO estimates of funding for inpatient and outpatient care for people treated for drug-susceptible TB, which are based on WHO estimates of the unit costs of bed-days and visits combined with the average number of outpatient visits and bed-days per TB patient as reported by NTPs.
c The category of drug-resistant TB includes funding reported by NTPs for the following items: anti-TB drugs required for treatment of multidrug and rifampicin-resistant TB (MDR/RR-TB, which includes people with pre-extensively drug-resistant TB and extensively drug-resistant TB, XDR-TB); any programme management (staff and activity) costs specifically required for the provision of care to people with drug-resistant TB; and WHO estimates of funding for inpatient and outpatient care. The categories for which funding is reported to WHO do not allow for funding for the diagnosis of drug-resistant TB specifically to be distinguished. In data analysis, the category of laboratory supplies and equipment is allocated to drug-susceptible TB. Rapid tests recommended by WHO can detect TB and RR-TB simultaneously.
d Data for TB preventive treatment (drugs only) are only available from 2019 onwards.
Fig. 4.1.7 Funding available for drug-susceptible TB and drug-resistant TB in three country groups, 2015–2024
a BRICS is used to refer only to the five original members of the BRICS group of countries, acknowledging that this group expanded in 2024 and in 2025 comprises 11 countries.
b The two global TB watchlist countries included are Cambodia and Zimbabwe.
c The category of drug-susceptible TB includes funding reported by NTPs for the following items: laboratory equipment and supplies; anti-TB drugs; programme management (including staff and activities); operational research and surveys; patient support; and miscellaneous items. It also includes WHO estimates of funding for inpatient and outpatient care for people treated for drug-susceptible TB, which are based on WHO estimates of the unit costs of bed-days and visits combined with the average number of outpatient visits and bed-days per TB patient as reported by NTPs.
d The category of drug-resistant TB includes funding reported by NTPs for the following items: anti-TB drugs required for treatment of multidrug and rifampicin-resistant TB (MDR/RR-TB, which includes people with pre-extensively drug-resistant TB and extensively drug-resistant TB, XDR-TB); any programme management (staff and activity) costs specifically required for the provision of care to people with drug-resistant TB; and WHO estimates of funding for inpatient and outpatient care. The categories for which funding is reported to WHO do not allow for funding for the diagnosis of drug-resistant TB specifically to be distinguished. In data analysis, the category of laboratory supplies and equipment is allocated to drug-susceptible TB. Rapid tests recommended by WHO can detect TB and RR-TB simultaneously.
Funding gaps for implementation of national strategic plans for TB
Data about required budgets and expected funding for the implementation of national strategic plans for TB, and associated sources of funding, are reported to WHO by NTPs as part of WHO’s annual rounds of global TB data collection. Funding gaps, as identified by NTPs, were estimated based on the difference between (i) the required budget and (ii) the expected level of funding.
In 2025, 52 of the 131 LMICs reported that funding was not sufficient for full implementation of their national strategic plans for TB (Fig. 4.1.8).
Fig. 4.1.8 The 131 low- and middle-income countriesa that did and did not report funding gaps for full implementation of their national strategic plans for TB in 2025

The combined total of the funding gaps reported by 52 countries for 2025 amounted to US$ 1.6 billion. The largest gaps were reported by countries in the African and Western Pacific regions. In terms of country income groups, the largest gap was reported by lower-middle-income countries; US$ 1.0 billion in 2025, a drop from US$ 1.1 billion in 2024. Of the 26 LICs, 14 (54%) reported funding gaps that amounted to US$ 233 million in 2025 (Fig. 4.1.9).
Fig. 4.1.9 Gaps between the funding required for national strategic plans for TB and the expected level of funding as reported by national TB programmes,a by income group and by WHO region, 2015–2025
Focusing on data from the 30 high TB burden countries and three global TB watchlist countries, Nigeria (US$ 290 million), Bangladesh (US$ 237 million), Indonesia (US$ 185 million), Viet Nam (US$ 139 million) and Kenya (US$ 94 million) reported the largest funding gaps (Fig. 4.1.10).
Fig. 4.1.10 Sources of expected fundinga and funding gaps reported for the TB-specific budgets included in national strategic plans for TB in the 30 high TB burden countries and three global TB watchlist countries,b 2025c
b The three global TB watchlist countries are Cambodia, the Russian Federation and Zimbabwe; for further details, see Annex 3 of the core report document.
c Four countries i.e. Angola, the Democratic People’s Republic of Korea, Liberia and Sierra Leone had not reported budget data for 2025 to WHO at the time the data snapshot for this webpage was taken (30 July 2025).
d In the most recent classification of countries by income group published by the World Bank (11), the Russian Federation was categorized as a high-income country. It was included as an upper-middle-income country because it was an upper-middle-income country for most of the period 2015–2024, is in WHO’s list of high burden countries for drug-resistant TB and is one of the three countries in WHO’s list of global TB watchlist countries (having been in WHO’s list of high TB burden countries until 2020). For more details about WHO’s lists of high burden countries for TB, drug-resistant TB and TB/HIV, see Annex 3 of the core report document.
The Stop TB Partnership’s Global Plan to End TB (the Global Plan) for 2023–2030 estimated global funding needs of US$ 15–32 billion per year in LMICs. The estimated funding needed in 2025 was US$ 20 billion, of which US$ 2.3 billion was in LICs, US$ 11 billion was in lower-middle-income countries and US$ 6.0 billion was in upper-middle-income countries (6).
Overall, the total required budget reported by LMICs to WHO represented only 39% of the estimated needs for LMICs in 2025 in the Global Plan (Fig. 4.1.11). A likely explanation is that national strategic plans for TB are much less ambitious (in scale and scope) than the Global Plan. National plans will be influenced by known resource constraints, in terms of the funding available domestically and from international sources.
As an example, the reported funding gap in LICs (US$ 0.23 billion) is only around 12% of the gap (US$ 2.0 billion) between the estimated needs in the Global Plan for LICs (US$ 2.3 billion) and their expected level of funding in 2025 (US$ 0.33 billion) (6).
Fig. 4.1.11 Gaps between the funding required for national strategic plans for TB as reported by NTPsa and the estimated funding needs in the Global Plan, by income group, 2025
Increases in both domestic and international funding for TB
are urgently required. Variation in the share of funding from domestic
sources within a given income group suggests that there is scope to
increase domestic funding in some high TB burden and global TB watchlist
countries. The need for increases in domestic funding has become even
more pressing, in the context of substantial changes to the
international donor funding landscape in early 2025. Until 2024,
allocations by The Global Fund and its major donor, the US government
(also the leading bilateral donor for TB), were the dominant influences
on international donor funding for TB (see also Section
4.2 of this report).
Estimated cost per person treated for TB
The median cost per person treated for TB in 2024, from a provider perspective, was US$ 797 for drug-susceptible TB (Fig. 4.1.12).
Fig. 4.1.12 Estimated cost per person treated for drug-susceptible TBa compared with GDP per capita in 117 countries,b 2024
Red dots indicate the 30 high TB burden and three global TB watchlist countries, blue dots indicate other countries; the size of each dot is proportional to the number of national notifications of people diagnosed with drug-susceptible TB in 2024. Put cursor over a dot to see the country name and data.
b Limited to countries with at least 100 people on first-line treatment in 2024 and that reported funding and utilisation data to WHO.
The median cost per person treated for drug-resistant TB, from
a provider perspective, was US$ 4232 in 2024
(Fig. 4.1.13). These
amounts include all of the provider costs associated with treatment and
TB programme-related costs. Importantly, the median cost fell by around
US$ 600 between 2023 and 2024; the likely explanation is expanded use of
6-month treatment regimens (first recommended by WHO in 2022) (Fig.
2.4.10 of Section
2.4).
In a few countries, the cost per person treated has fallen by around
US$ 500–1000 (e.g. Indonesia, Pakistan, Ukraine).
Fig. 4.1.13 Estimated cost per person treated for drug-resistant TBa compared with GDP per capita in 87 countries,b 2024
Red dots indicate the 30 high MDR/RR-TB burden countries, blue dots indicate other countries; the size of each dot is proportional to the number of national notifications of people diagnosed with drug-resistant TB in 2024. Put cursor over a dot to see the country name and data.
a The following costs are included: anti-TB drugs; programme management (staff and activity) costs specifically required for the provision of care to people with drug-resistant TB; inpatient and outpatient care.
b Limited to countries with at least 20 people on second-line treatment in 2024 and that reported funding and utilisation data to WHO.
Estimates of the costs incurred by people with TB and their
households during diagnosis and treatment are available from national
surveys (Section
5.2).
Further details about funding for TB prevention, diagnostic and treatment services are available in country profiles and the Global Tuberculosis Report mobile app. Methods for data collection and analysis are summarized below (Box 4.1).
Data shown on this webpage are as of 30 July 2025 (see Annex 2 of the core report document for more details).
Box 4.1
Methods used to compile, review, validate and analyse financial data reported to WHO
WHO began monitoring government and international donor financing for TB prevention, diagnostic and treatment services in 2002. All data are stored in the WHO global TB database. The standard methods used to compile, review, validate and analyse these data are described in detail in a technical appendix; this box provides a summary.
The methods used to systematically review and validate data have remained consistent since 2002. They include routine checks for plausibility and consistency, and discussions with country respondents to resolve queries. In reviewing and validating data, particular attention has always been given to high TB burden countries.
Missing data are handled as follows:
The analysis of available funding for TB uses reported information on received funding. When received funding is not available for a given year, expenditure data are used. If data on received funding and expenditure are both unavailable, data on committed funds are used. If none of these data are available, received funding, expenditure or committed funds from adjacent years are used. For analysis of funding in 2024, received funding was replaced by one of these methods for 33 countries, which collectively accounted for 4.2% of the global number of notified cases of TB in 2024 (this included five high burden countries, Angola, Liberia, Papua New Guinea, the Democratic People’s Republic of Korea and Sierra Leone, which in combination accounted for 2.8% of the global number of TB case notifications). Nine countries (collectively accounting for 0.50% of the global number of notified cases of TB in 2024) did not have sufficient data for any of the above methods to be applied; the estimated financial costs associated with inpatient and outpatient treatment were the only components included for these countries, using the methods described below.
When the breakdown of received funding by source or by category is missing for a given year, country-specific shares from the previous year are applied instead.
Since TB funding reported by NTPs does not usually include the financial costs associated with the inpatient and outpatient care required during TB treatment (exceptions among high TB or MDR/RR-TB burden countries include Belarus, China, Kazakhstan and the Russian Federation), country-specific estimates of the funding required for both inpatient and outpatient care are added. This is done by multiplying the reported number of TB patients notified by the product of the average number of bed days and outpatient visits per patient (as reported by NTPs) and their respective unit costs; this is done separately for TB patients with drug-susceptible TB and drug-resistant TB. Unit costs are estimated using the WHO CHOosing Interventions that are Cost-Effective (WHO-CHOICE) methods (15).
Trend data are shown in constant (as opposed to current) 2024 US
dollars. In other words, funding amounts are shown in real terms, after
adjustment for inflation. Figures and tables that show data for 2024
only are labelled as current 2024 US dollars.
References
Floyd K, Fitzpatrick C, Pantoja A, Raviglione M. Domestic and donor financing for tuberculosis care and control in low-income and middle-income countries: an analysis of trends, 2002–11, and requirements to meet 2015 targets. Lancet Glob Health. 2013;1(2):e105–15 (https://doi.org/10.1016/s2214-109x(13)70032-9).
Floyd K, Pantoja A, Dye C. Financing tuberculosis control: the role of a global financial monitoring system. Bull World Health Organ. 2007;85(5):334–40 (https://doi.org/10.2471/blt.06.034942).
Su Y, Garcia Baena I, Harle AC, Crosby SW, Micah AE, Siroka A et al. Tracking total spending on tuberculosis by source and function in 135 low-income and middle-income countries, 2000-17: a financial modelling study. Lancet Infect Dis. 2020;20:929-42 (https://doi.org/10.1016/S1473-3099(20)30124-9).
Treatment Action Group, Stop TB Partnership. Tuberculosis research funding trends 2005–2023. New York: Treatment Action Group; 2024 (https://www.treatmentactiongroup.org/wp-content/uploads/2024/12/TB_funding_2024_final.pdf).
Resolution 78/5: Political declaration of the high-level meeting of the General Assembly on the fight against tuberculosis. New York: United Nations; 2023 (https://undocs.org/A/RES/78/5).
The Global Plan to End TB, 2023–2030. Geneva: Stop TB Partnership; 2022 (https://www.stoptb.org/global-plan-to-end-tb/global-plan-to-end-tb-2023-2030).
Cavalcanti DM, de Oliveira Ferreira de Sales L, da Silva AF, Basterra EL, Pena D, Monti C et al. Evaluating the impact of two decades of USAID interventions and projecting the effects of defunding on mortality up to 2030: a retrospective impact evaluation and forecasting analysis. Lancet. 2025;406:283-94 (https://doi.org/10.1016/S0140-6736(25)01186-9).
Clark RA, McQuaid CF, Richards AS, Bakker R, Sumner T, Prys-Jones TO et al. The potential impact of reductions in international donor funding on tuberculosis in low-income and middle-income countries: a modelling study. Lancet Glob Health. 2025;13:e1517-e24 (http://doi.org/10.1016/S2214-109X(25)00232-3).
Mandal S, Nair S, Sahu S, Ditiu L, Pretorius C. A deadly equation: The global toll of US TB funding cuts. PLOS Glob Public Health. 2025;5:e0004899 (http://doi.org/10.1371/journal.pgph.0004899).
Stover J, Sonneveldt E, Tam Y, Horton KC, Phillips AN, Smith J et al. Effects of reductions in US foreign assistance on HIV, tuberculosis, family planning, and maternal and child health: a modelling study. Lancet Glob Health. 2025;13(10):e1669-e80 (https://doi.org/10.1016/S2214-109X(25)00281-5).
World Bank Country and Lending Groups. New York: World Bank; 2025 ( https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups).
Global Tuberculosis Report 2024. Geneva: World Health Organization; 2024 (https://iris.who.int/handle/10665/379339). License: CC BY-NC-SA 3.0 IGO.
The Global Fund; Geneva: (https://www.theglobalfund.org/en/).
Green A. Global Fund plans to cut US$1.4 billion from grants it has already awarded. Devex. 10 July 2025. Available from: https://www.devex.com/news/global-fund-plans-to-cut-1-4-billion-from-grants-it-has-already-awarded-110481 [cited 27 August 2025].
Stenberg K, Lauer JA, Gkountouras G, Fitzpatrick C, Stanciole A. Econometric estimation of WHO-CHOICE country-specific costs for inpatient and outpatient health service delivery. Cost Eff Resour Alloc. 2018;16:11 (https://doi.org/10.1186/s12962-018-0095-x).
Organisation for Economic Co-operation and Development, Eurostat and World Health Organization (2017). A System of Health Accounts 2011: Revised edition. Paris: OECD Publishing; 2017 (http://dx.doi.org/10.1787/9789264270985-en).
General disclaimers
The designations employed
and the presentation of the material in this publication do not imply
the expression of any opinion whatsoever on the part of WHO concerning
the legal status of any country, territory, city or area or of its
authorities, or concerning the delimitation of its frontiers or
boundaries. Dotted and dashed lines on maps represent approximate border
lines for which there may not yet be full agreement.
