
2.1 Case notifications
Tuberculosis (TB) case notifications refer to people diagnosed with TB disease and officially reported as a case to national authorities. Case notification data have been systematically collected at national level and then reported to WHO on an annual basis since the mid-1990s, based on standard case definitions and associated guidance on the recording and reporting of data provided by WHO. The most recent WHO guidance was published in 2024 (1).
Globally in 2024, 8.3 million people were diagnosed with a new episode of TB (also referred to as new and recurrent cases) and notified (Table 2.1.1). Of these, 84% had pulmonary TB and 16% had extrapulmonary TB. Three WHO regions accounted for 87% of total notifications: the African Region (23%), South-East Asia Region (38%) and Western Pacific Region (26%). In 106 countries that accounted for 87% of global notifications, 15% of people newly diagnosed with TB were reported to have been detected through screening (for further details, see Section 3).
Table 2.1.1 Case notifications of people diagnosed with TB, MDR/RR-TB and XDR-TB, globally and for WHO regions, 2024
| WHO region | Total notified | New and recurrenta | Pulmonary new and recurrent number | Pulmonary new and recurrent bacteriologically confirmed (%) | Extrapulmonary new and recurrent (%) | People living with HIV, new and recurrent | MDR/RR-TB onlyb | Pre-XDR-TB or XDR-TBc |
|---|---|---|---|---|---|---|---|---|
| African Region | 1 971 436 | 1 931 363 | 1 709 832 | 70% | 11% | 291 294 | 20 730 | 1089 |
| Region of the Americas | 284 484 | 259 194 | 224 356 | 81% | 13% | 25 143 | 5878 | 334 |
| South-East Asia Region | 3 264 399 | 3 134 998 | 2 366 649 | 64% | 25% | 45 458 | 52 865 | 8909 |
| European Region | 160 679 | 139 608 | 115 704 | 70% | 17% | 16 252 | 26 453 | 10 689 |
| Eastern Mediterranean Region | 672 749 | 664 741 | 512 006 | 55% | 23% | 2025 | 4833 | 1482 |
| Western Pacific Region | 2 223 054 | 2 174 780 | 2 008 045 | 59% | 8% | 33 344 | 36 833 | 2637 |
| Global | 8 576 801 | 8 304 684 | 6 936 592 | 64% | 16% | 413 516 | 147 592 | 25 140 |
b RR-TB, rifampicin-resistant TB; MDR-TB, multidrug-resistant TB (defined as TB that is resistant to rifampicin and isoniazid). This column excludes any cases with known resistance to any fluoroquinolone.
c XDR-TB, extensively drug-resistant TB. Pre-XDR-TB is defined as TB that is resistant to rifampicin and to any fluoroquinolone. XDR-TB is TB that is resistant to rifampicin and to any fluoroquinolone, and to at least one of bedaquiline or linezolid.
The 8.3 million people newly diagnosed with TB and notified as a TB case in 2024 was a small increase from 8.2 million in 2023, following the large increases that occurred between 2021 and 2023 as countries recovered from major COVID-related disruptions to TB diagnosis and treatment in 2020 (Fig. 2.1.1).
The historically high numbers in 2022, 2023 and 2024 can be explained by two factors: the diagnosis of a backlog of people who developed TB in previous years but whose diagnosis was delayed by COVID-related disruptions, and a rise in the overall number of people developing TB disease between 2020 and 2023 as a result of increased transmission resulting from diagnostic delays (Section 1.1).
Fig. 2.1.1 Global trend in case notifications of people newly diagnosed with TB, 2010–2024
Trends in case notifications since the pre-pandemic year of 2019 vary among the six WHO regions (Fig. 2.1.2). The pattern in the Eastern Mediterranean and South-East Asia regions was very similar to the global trend, with a big reduction in 2020 followed by year-on-year increases from 2021–2024: the South-East Asia Region drove the global trend. The pattern was also similar in the Region of the Americas, the European Region and the Western Pacific Region; the main difference is that in these three regions, notifications fell between 2023 and 2024. In the African Region, notifications fell only slightly in 2020 and subsequently in the African Region increased, particularly between 2021 and 2023, before levelling off in 2024. In 2024, the reported number of people newly diagnosed with TB in the African Region was 38% above the level of 2019.
Fig. 2.1.2 Regional trends in case notifications of people newly diagnosed with TB, 2010–2024
In most of the 30 high TB burden countries and three global TB
watchlist countries, case notifications fell in 2020 and have
subsequently recovered to the pre-COVID level or beyond
(Fig. 2.1.3).
Exceptions to this general pattern include three countries where
notifications increased throughout the period 2019–2024 (the Central
African Republic, the Democratic Republic of the Congo and Nigeria) and
three countries where a long-term historic decline continued largely
uninterrupted (China, the Democratic People’s Republic of Korea and the
Russian Federation). Two other exceptions are Ethiopia and Zimbabwe,
where a relatively consistent decline for several years has been
reversed since 2021 and 2020 respectively. In Ethiopia, recent increases
may reflect active case finding efforts. In Zimbabwe, recent increases
may reflect an underlying increase in TB incidence.
Fig. 2.1.3 Case notifications of people newly diagnosed with TB in the 30 high TB burden and three global TB watchlist countries, 2010–2024
Most notified cases of TB are among adults
(Fig. 2.1.4). Of the
global total of people notified as a new or recurrent TB case in 2024,
55% were men, 36% were women and 8.3% were children aged 0–14 years (the
age groups related to children for which WHO routinely collects data are
0–4 and 5–14 years; it is recognized that the second category includes
young adolescents). For the remainder, either age or sex were unknown.
In general, notification data appear to understate the share of the
total TB disease burden that is accounted for by men, since higher male
to female ratios among adults have been found in national TB prevalence
surveys (Section
1.4). The drop in case
notifications between 2019 and 2020 and subsequent recovery was similar
for men and women, while both the drop in 2020 and subsequent recovery
were more pronounced for children.
Fig. 2.1.4 Global trend in case notifications of people newly diagnosed with TB disaggregated by age and sex, 2013–2024a
Although the global proportion of notified cases accounted for
by children aged 0–14 years has been relatively stable (7–8% of the
total notifications) (Fig.
2.1.4), there is considerable variation at country level
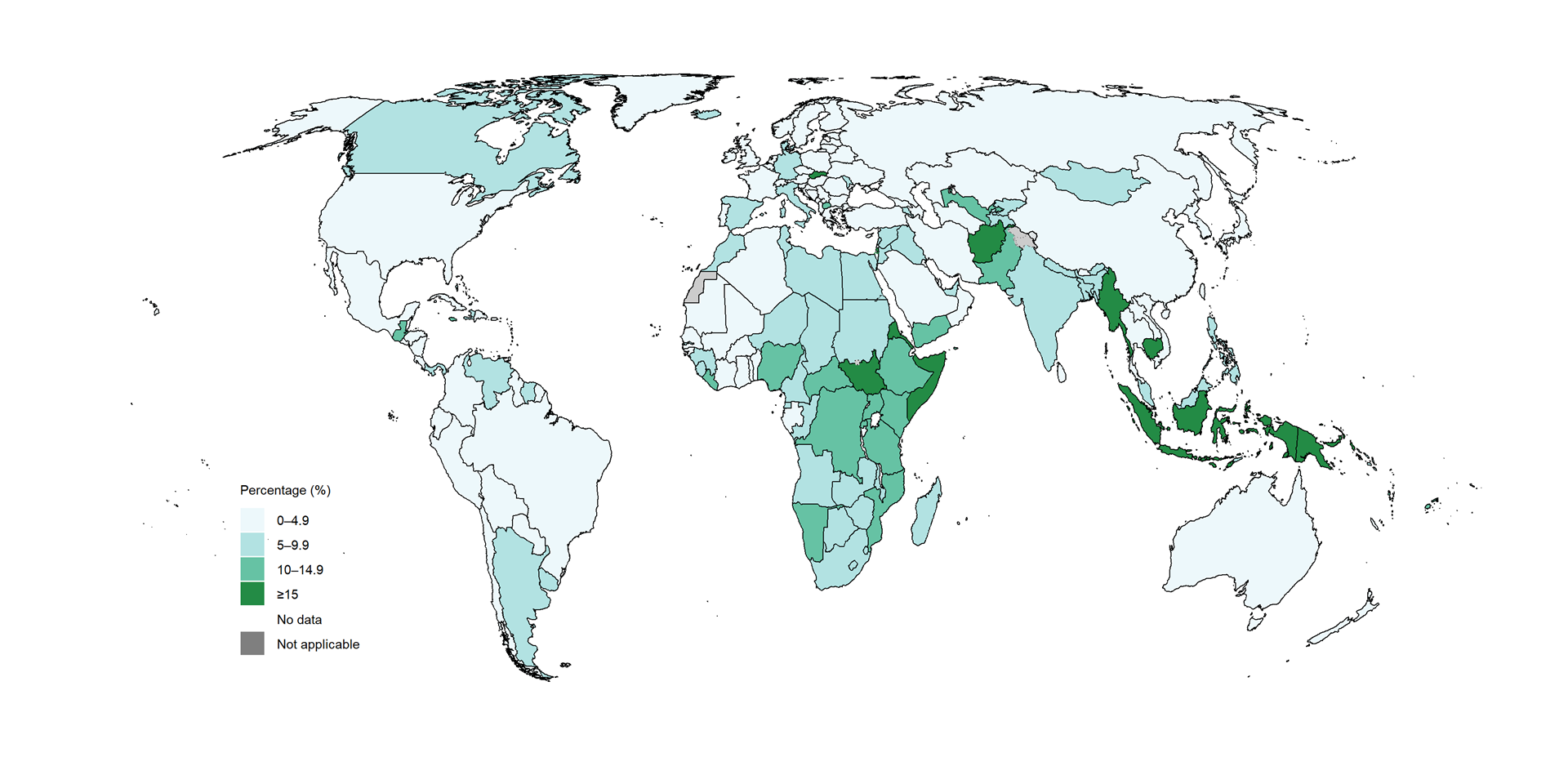
(Fig. 2.1.5). Among
the 30 high burden countries, those with particularly low levels
(<5%) included Brazil, China, Gabon, Liberia, the Democratic People’s
Republic of Korea, Thailand and Viet Nam.
There are recognized issues with the diagnosis and reporting of TB in children, including the use of variable case definitions and underreporting of cases diagnosed by paediatricians in the public and private sectors. Greater attention to the quality of TB notification data for children is warranted in many countries.
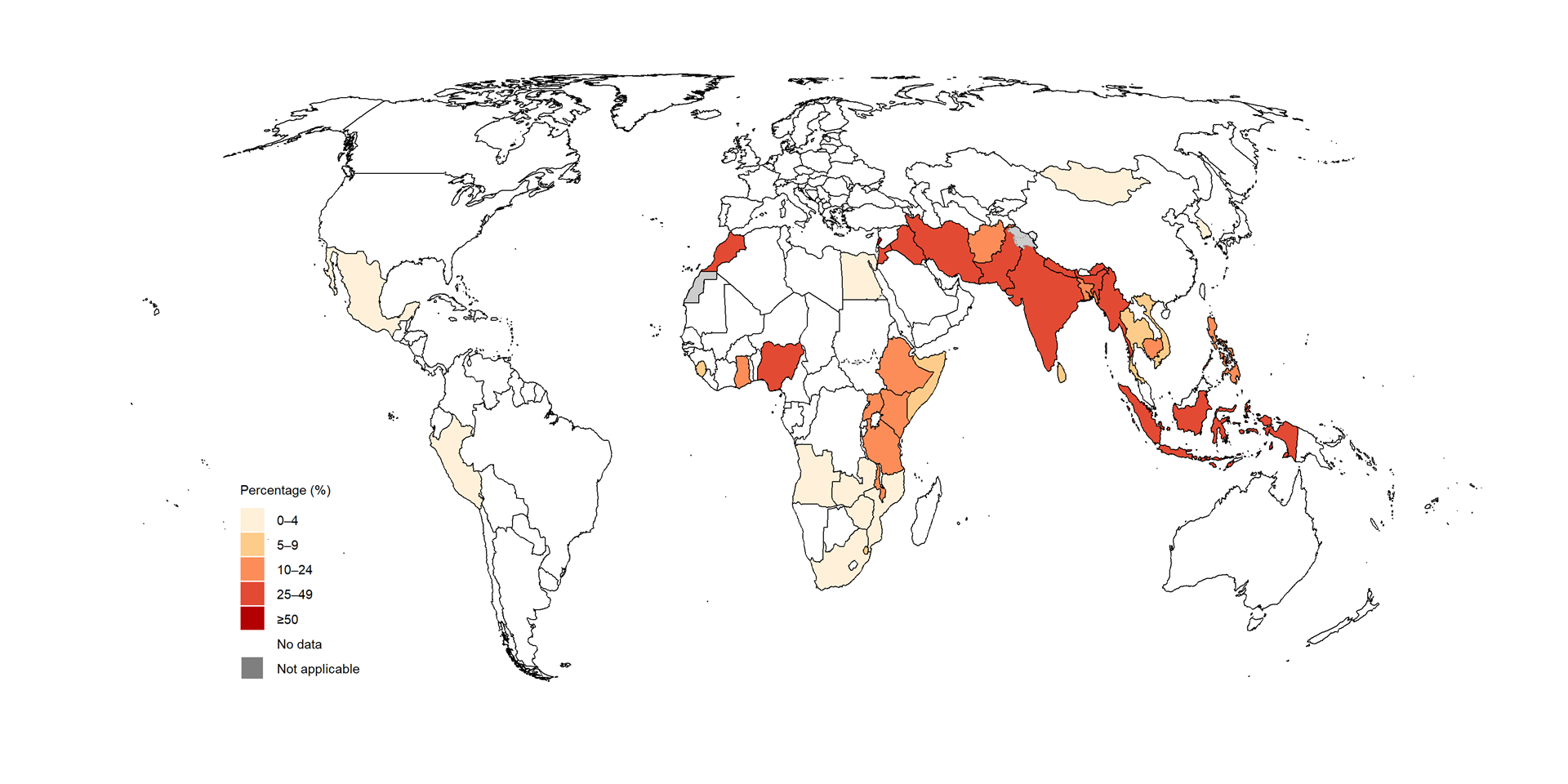
Fig. 2.1.5 Percentage of people notified as a new or recurrent case of TB who were aged 0–14 years,a by country, 2024
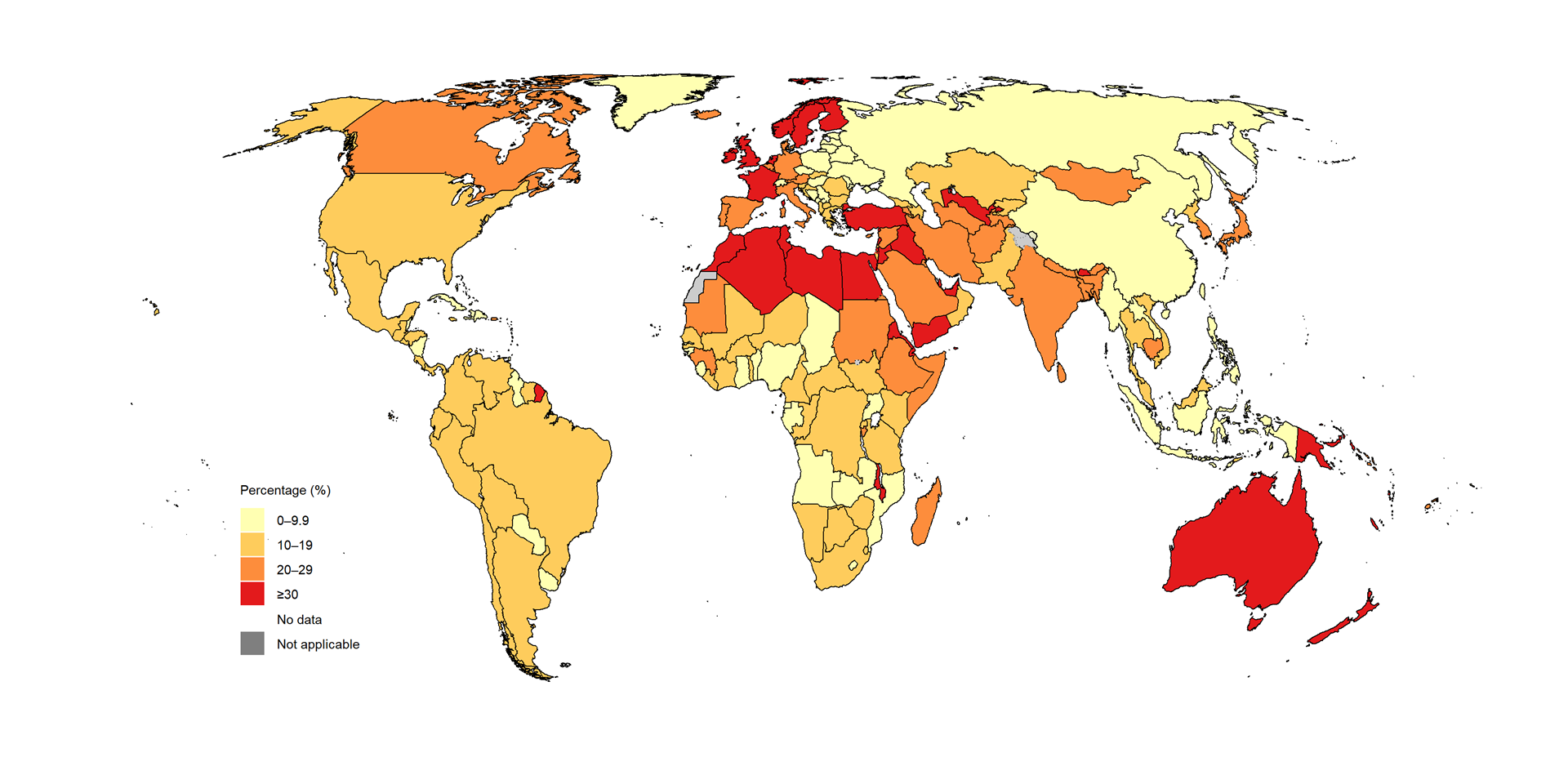
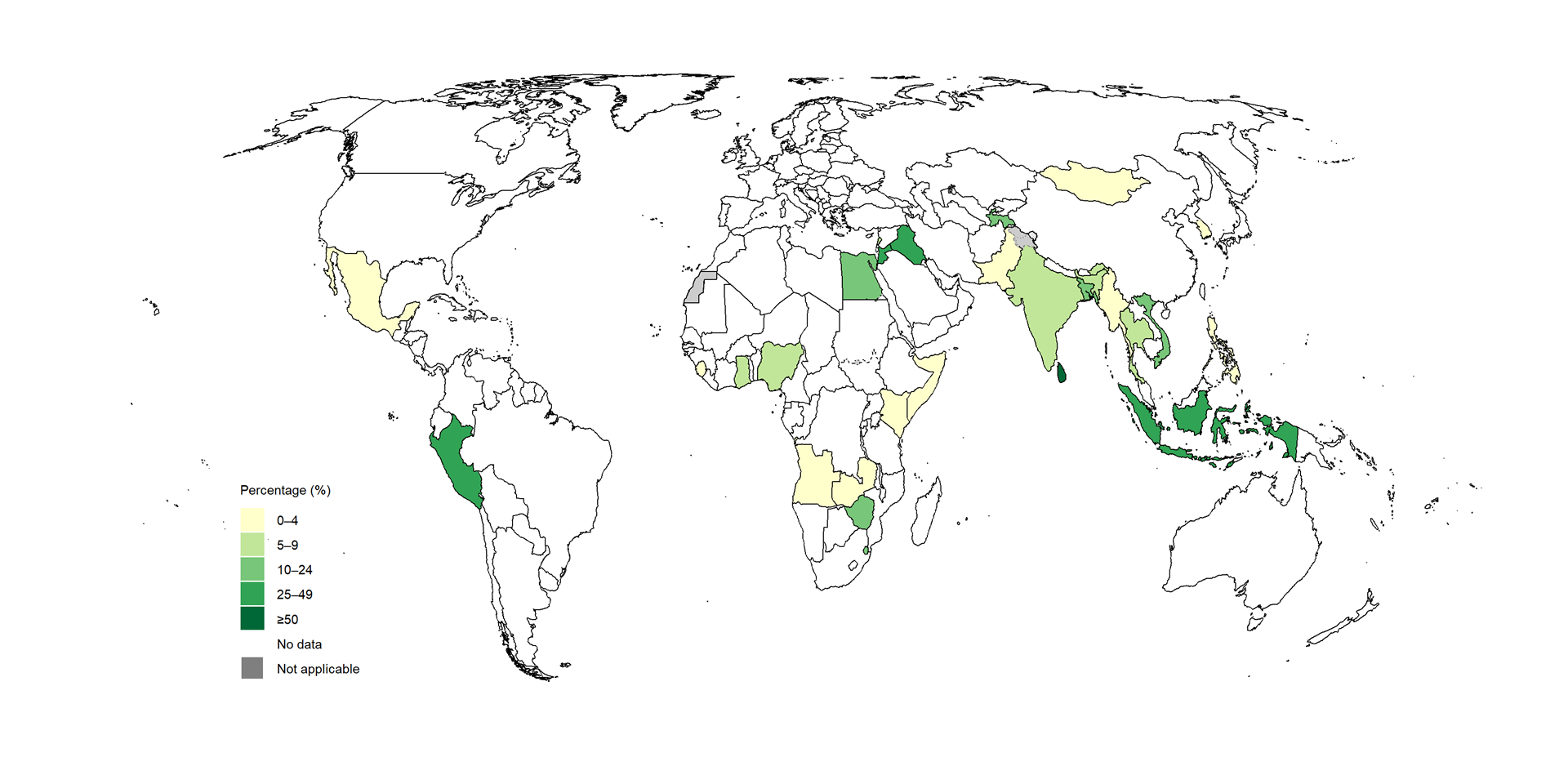
There is also considerable country variation in the proportion of notified cases diagnosed with extrapulmonary TB (Fig. 2.1.6). This may reflect underlying differences in TB epidemiology as well as diagnostic practices.
Among the 30 high TB burden and three global TB watchlist countries, the share of case notifications accounted for by people diagnosed with extrapulmonary TB was particularly high (>20%) in Bangladesh, Ethiopia, India, Cambodia, Mongolia and Papua New Guinea. Even higher proportions were reported in some other parts of the world; examples included Australia, Finland, France, Ireland, the Netherlands, New Zealand, Norway, Sweden, Türkiye, the United Kingdom of Great Britain and Northern Ireland, Uzbekistan and several countries in the WHO Eastern Mediterranean Region.
Fig. 2.1.6 Percentage of people notified as a new or recurrent case of TB who were diagnosed with extrapulmonary TB, by country, 2024
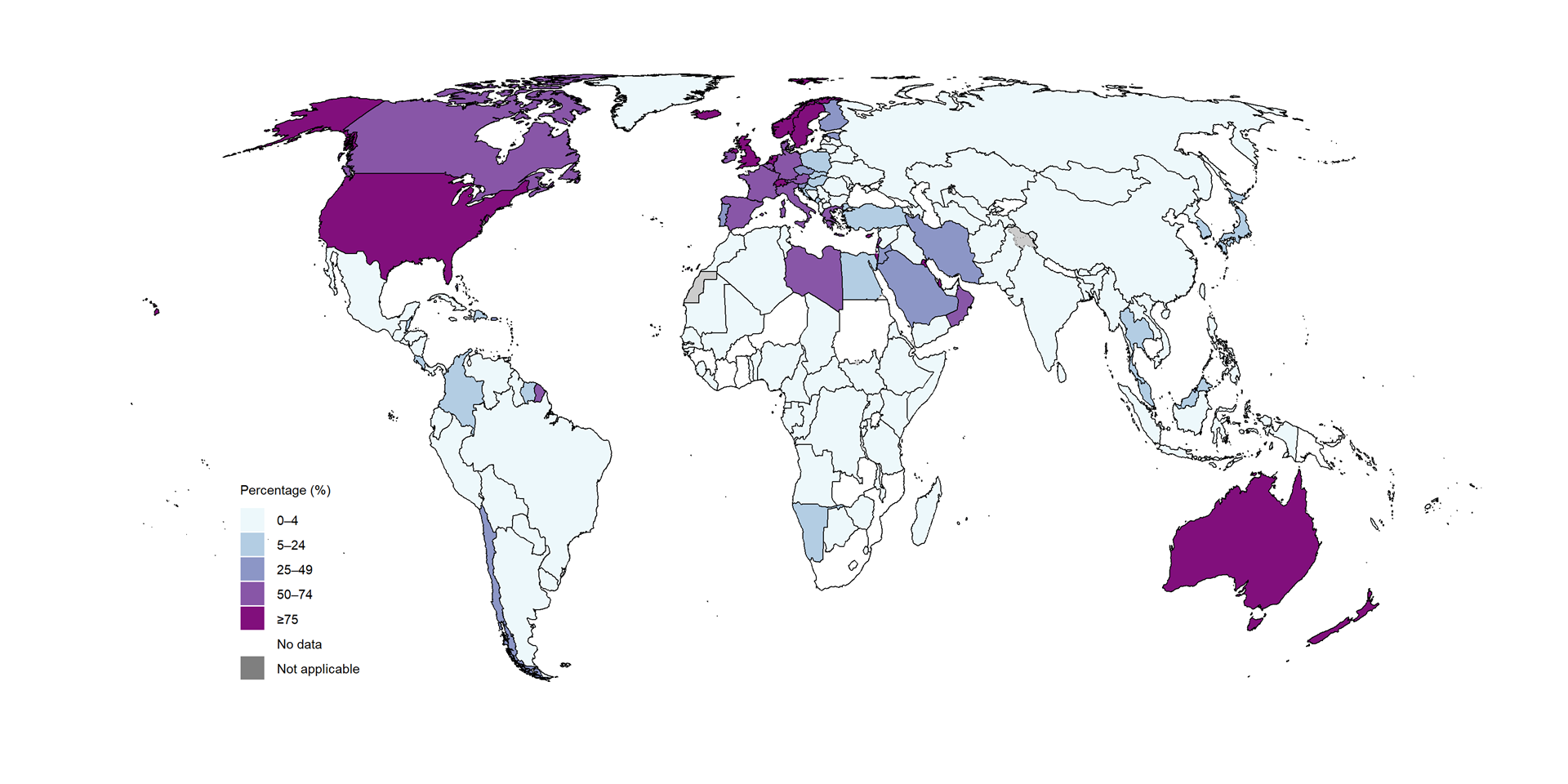
There is striking country variation in the distribution of TB
case notifications according to country of origin
(Fig. 2.1.7). In
several countries with a low incidence of TB (Section
1.1), more than 75% of notified
cases were among people of foreign origin.
Fig. 2.1.7 Percentage of people notified as a TB case (new, recurrent or re-registereda for treatment) who were of foreign origin, by country, 2024
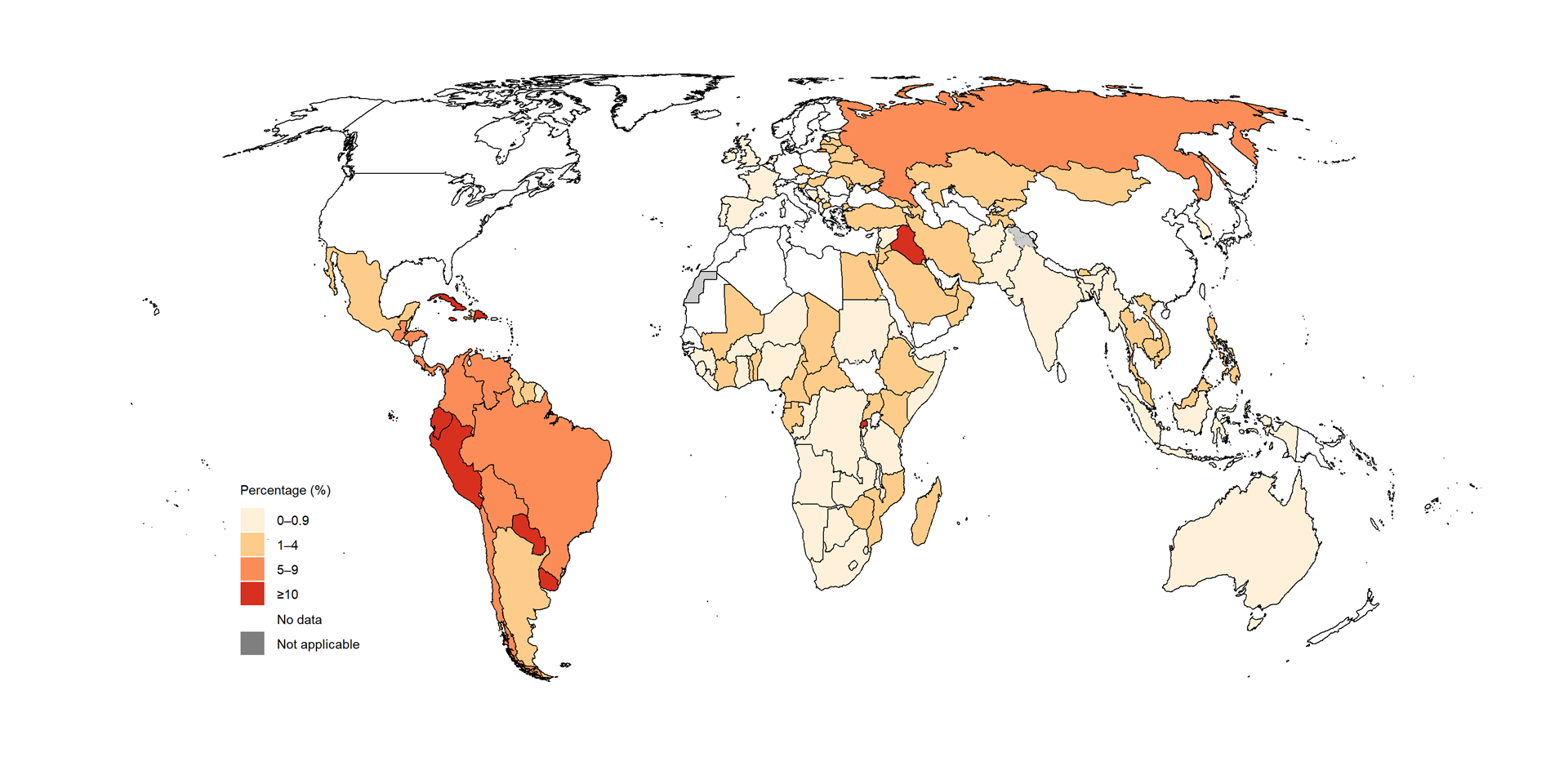
People housed in prisons or congregate settings have a high risk of developing TB and of having poorer TB treatment outcomes than the general population. Prisons can exacerbate ill health: for example, if there is chronic lack of investment in the justice sector, contraventions of human rights, low prioritization of health and harm reduction services in prisons, and an absence of other justice-based alternatives to incarceration. The physical infrastructure of prisons, including the risk of overcrowding and the frequent movement of prisoners can increase the risk of transmitting airborne diseases such as TB.
Data about the number of people notified as a new or recurrent case of TB who were registered in prisons have been collected from all countries in the WHO European Region since 2014 and from all countries in the Region of the Americas since 2018. Data have been requested from all countries and areas (n=215) since in 2023; 141 countries and areas reported data. These data reveal considerable country variation in the percentage of people notified as a new and recurrent case of TB who were registered in prisons (Fig. 2.1.8), with the highest percentages are in countries and areas in the Region of the Americas.
Fig. 2.1.8 Percentage of people notified as a new and recurrent case of TB who were registered in prisons, by country, 2024
Engagement of all care providers in the public and private
sectors through public–private and public–public mix (PPM) initiatives
can help to minimize the underreporting of people diagnosed with TB.
Since 2015, the contribution of such PPM initiatives to total
notifications has grown in most of the seven countries defined as top
global priorities for PPM (Fig.
2.1.9).
Fig. 2.1.9 Contribution of public-privatea mix and public-publicb mix initiatives to case notifications of people diagnosed with TB in seven global priority countries, 2010–2024
b Public-public mix refers to engagement by the NTP with public health sector providers of TB care that are not under the direct purview of the NTP. Examples include public hospitals, public medical colleges, prisons and detention centres, military facilities and public health insurance organizations.
There is considerable country variation in the percentage of people notified as a TB case by public-private mix and public-public initiatives (Fig. 2.1.10).
Fig. 2.1.10 Percentage of people notified as a TB case by public-privatea mix and public-publicb initiatives, by country,c 2024
a) Public-private mix initiatives
b) Public-public mix initiatives
b Public-public mix refers to engagement by the NTP with public non-NTP providers of TB care. Examples include public hospitals, public medical colleges, prisons/detention centres, military facilities, railways and public health insurance organizations.
c In 2024, WHO requested 42 countries to report data about the number of people notified as a TB case through public-private and public-public mix initiatives, of which 37 countries did so.
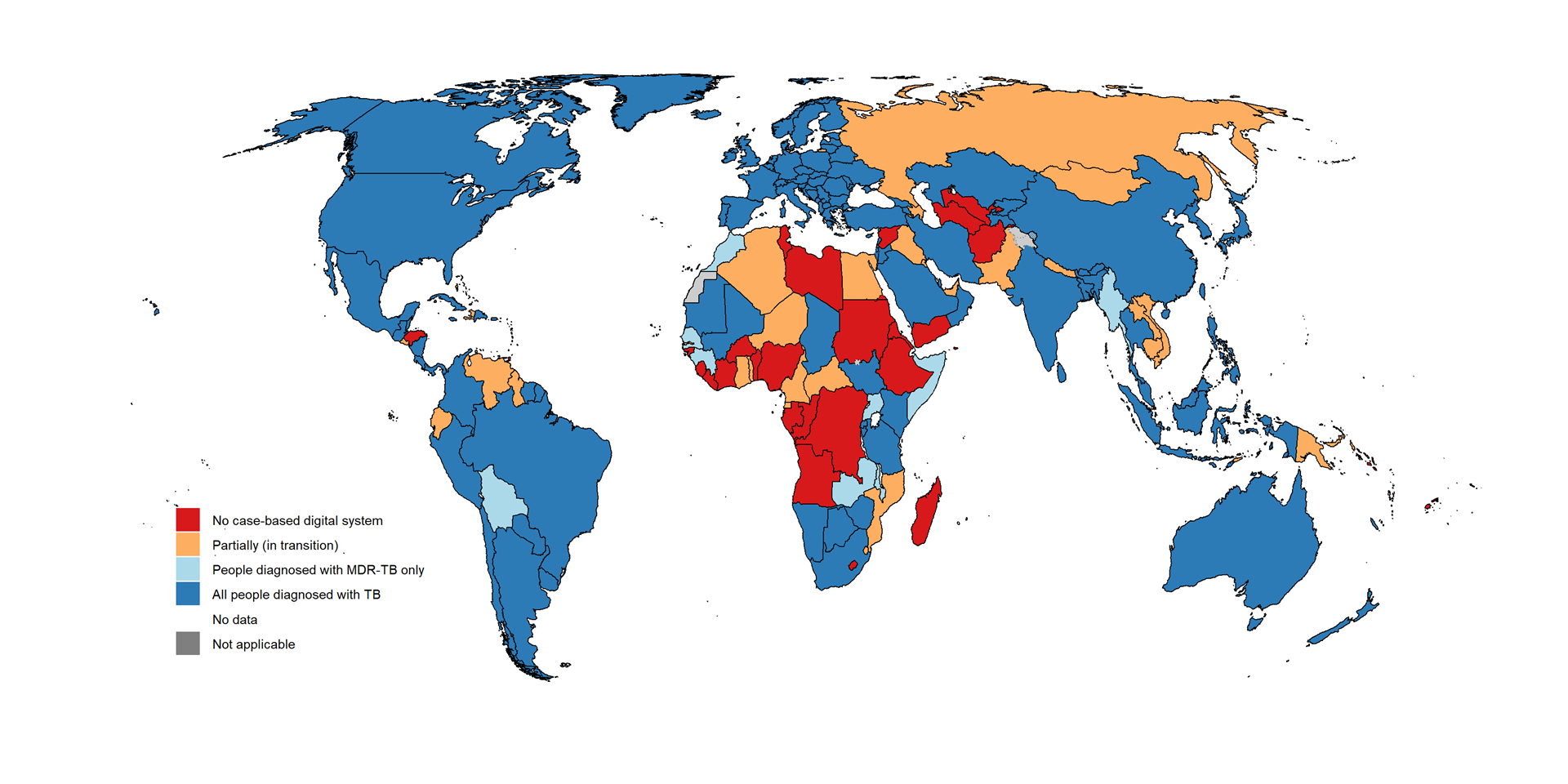
Case-based digital surveillance systems enable timely reporting and use of TB data; their main advantages are highlighted in the latest WHO guidance on TB surveillance (1). In 2024, 129 countries and areas that collectively accounted for 69% of officially notified TB cases were using a case-based digital surveillance system that covered all people diagnosed with TB (Fig. 2.1.11). This was similar to the level of 2023, when 132 countries and areas that collectively accounted for 70% of officially notified TB cases were using such systems. Acceleration of progress in making the transition from paper-based reporting of aggregated TB data to case-based digital TB surveillance is particularly needed in the WHO African Region.
Fig. 2.1.11 Countries with national case-based digital surveillance systems for TB, 2024
Further country-specific details about TB case notifications
are available in the Global tuberculosis report app and country profiles.
Data shown on this webpage are as of 30 July 2025 (see Annex 2 of the core report document for more details).
Reference
- Consolidated guidance on tuberculosis data generation and use: module 1: tuberculosis surveillance. Geneva: World Health Organization; 2024 ( https://iris.who.int/handle/10665/376612). License: CC BY-NC-SA 3.0 IGO.
General disclaimers
The designations employed
and the presentation of the material in this publication do not imply
the expression of any opinion whatsoever on the part of WHO concerning
the legal status of any country, territory, city or area or of its
authorities, or concerning the delimitation of its frontiers or
boundaries. Dotted and dashed lines on maps represent approximate border
lines for which there may not yet be full agreement.
