
3. Tuberculosis prevention and screening
Preventing tuberculosis (TB) infection and stopping progression from infection to disease are critical for reducing TB incidence to the levels targeted by the End TB Strategy (1, 2). The main health care intervention to stop progression from infection to disease is TB preventive treatment (TPT), which the World Health Organization (WHO) recommends for people living with HIV, household contacts of people with TB and other risk groups (3, 4). Strategies to provide TPT are often linked to screening to find and treat people with TB earlier in the course of their disease and thus help to reduce transmission and improve outcomes (4). Other TB preventive approaches are TB infection prevention and control (5), food assistance for household contacts in food insecure settings (6, 7) and vaccination of children with the bacille Calmette-Guérin (BCG) vaccine. Addressing broader determinants that influence TB epidemics can also help to prevent TB infection and disease; these are discussed in Section 5.3.
3.1 TB preventive treatment
The global number of people living with HIV and household contacts of people diagnosed with TB who were provided with TPT increased from 1.0 million in 2015 to 3.6 million in 2019. There was then a sizeable reduction to 2.9 million in 2020 and 2021, probably reflecting disruptions to health services caused by the coronavirus (COVID-19) pandemic (Fig. 3.1). There was a substantial recovery to 3.9 million in 2022, above the pre-pandemic level. The total increased further in 2023 and reached 5.3 million in 2024.
Since 2021 there has been a particularly noticeable increase in the number of household contacts enrolled on TPT: from 0.76 million in 2021 to 3.5 million in 2024. In contrast, the number of people living with HIV who were enrolled on TPT increased between 2015 and 2019 (reaching a peak of 3.0 million in 2019) before falling in 2020 and subsequently levelling off at about 2 million people per year.
Fig. 3.1 Global number of people provided with TB preventive treatment (TPT), 2015–2024
At the second United Nations (UN) high-level meeting on TB in
2023, a new global target for TPT coverage was set
(8). The target is to
reach 90% coverage among people at high risk of developing TB disease by
2027; in absolute numbers, this is equivalent to providing TPT to up to
approximately 45 million people globally in the 5-year period 2023–2027,
including approximately 30 million household contacts of people with TB
and approximately 15 million people living with HIV.
TPT coverage has improved globally since 2015, but remained well below the target in 2024, for both household contacts (25%) and people living with HIV (58%) (Fig. 3.2). At regional level, there has been considerable progress since 2021 in TPT coverage among household contacts in the WHO African and South-East Asia regions.
Fig. 3.2 Trends in the coverage of TB preventive treatment (TPT), globally and by WHO region, 2015–2024
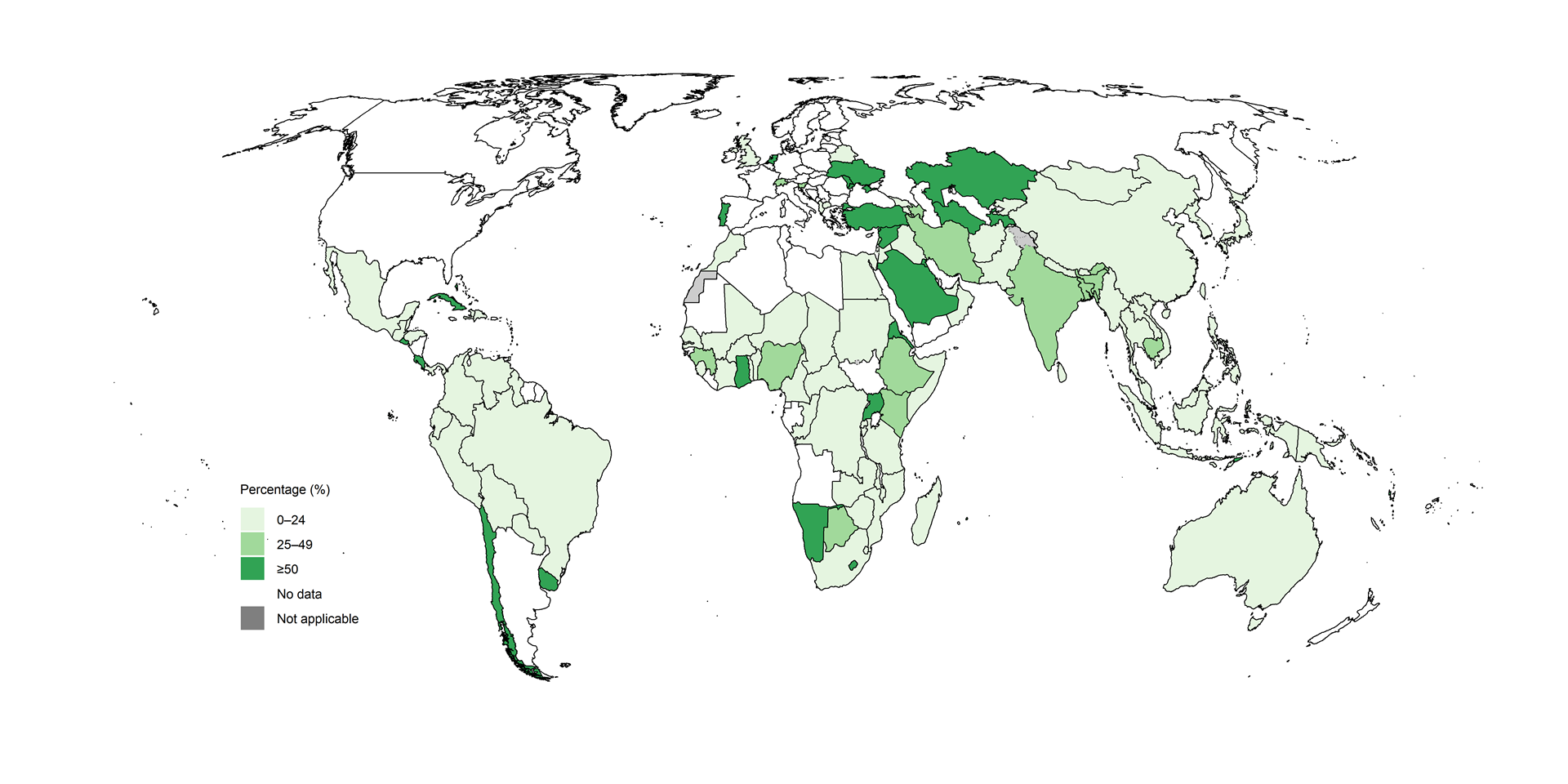
Ensuring access to shorter rifamycin-containing regimens may help to increase uptake of TPT. The number of people started on rifamycin-containing regimens increased steadily since 2022 in all WHO regions (Fig. 3.3). In 2024, 2.1 million people started shorter regimens in 88 countries, representing 45% of all people who started TPT in these countries that year. Among these 88 countries, 82 reported using the 3-month weekly regimen of rifapentine and isoniazid (3HP) and 28 reported using the 1-month daily regimen of rifapentine and isoniazid (1HP). Overall, 73% of people reported to have been initiated on rifamycin-based TPT in 2024 were using 3HP or 1HP and in 41 countries, 3HP or 1HP were used for 75% or more of people provided with rifamycin-based TPT (Fig. 3.4).
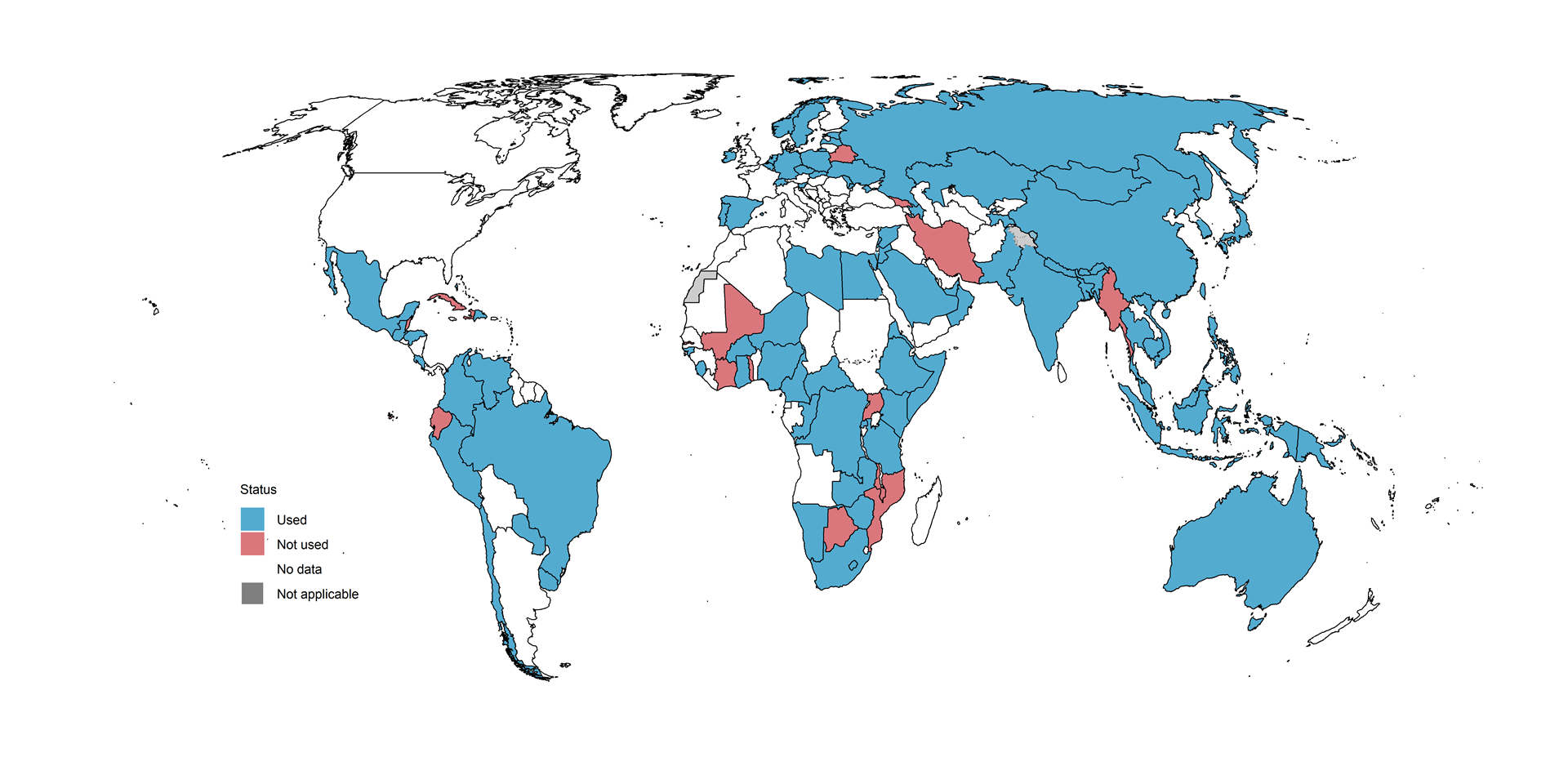
Rifampicin-based regimens were also being used in 2024: 86 countries reported using the 3-month daily regimen of rifampicin and isoniazid (3HR) and 51 reported using the 4-month daily regimen of rifampicin only (4R) (Fig. 3.5).
Fig. 3.3 Number of people started on TB preventive treatment using a rifamycin-containing regimen, globally and by WHO region, 2018–2024
Fig. 3.4 Percentage of people started on a rifamycin-containing TB preventive treatment regimen who were on a rifapentine-containing regimen (1HP or 3HP), by country, 2024

The regimen of 6 months of levofloxacin (6Lfx) for contacts of people with multidrug-resistant TB (MDR-TB), approved by WHO in 2024 (3), was used in 49 countries in 2024, including seven high TB burden countries (India, Indonesia, Mongolia, Mozambique, South Africa, Thailand and Zambia) and six high MDR-TB burden countries (Kazakhstan, Peru, the Republic of Moldova, the Russian Federation, Somalia and Ukraine) (Fig. 3.6).
Fig. 3.6 Countries using TB preventive treatment regimens containing levofloxacin (6Lfx), 2024

3.2 Household contacts
Globally in 2024, there were an estimated 14 million (95% uncertainty interval [UI]: 14–14 million) household contacts of people diagnosed with bacteriologically confirmed pulmonary TB. However, only 11 million contacts were reported in 2024 (up 14% from 9.3 million in 2023); 9.3 million (88%) of these contacts were evaluated for both TB infection and disease (up 18% from 7.9 million in 2023). The percentage of contacts who were evaluated varied widely among countries (Fig. 3.7).
A total of 2.8 million household contacts aged 5 years and over started TPT in 2024, representing a 45% increase compared with 2023 (Fig. 3.1). India accounted for over half of this increase.
In 2024, 0.65 million household contacts aged under 5 years started TPT out of an estimated 1.7 million who were eligible – almost unchanged (a 1.6% decrease) compared with 2023.
Globally, the 3.5 million household contacts provided with TPT in 2024 represented about 33% of the 11 million household contacts reported and 25% of the estimated total of 14 million household contacts. There was considerable variation among countries in both the percentage of household contacts who were evaluated for TB disease and infection, and the percentage of household contacts who were provided with TPT (Fig. 3.7, Fig. 3.8).
Fig. 3.7 Percentage of the reported number of household contacts of people newly diagnosed with bacteriologically confirmed pulmonary TB disease who were evaluated for TB disease and TB infection, by country, 2024

Data on completion of TPT among household contacts who started treatment in 2023 was reported by 95 countries; the median completion rate was 89% (interquartile range [IQR], 76–97%), but rates varied widely among WHO regions (Fig. 3.9).
Fig. 3.9 Completion of TB preventive treatment (TPT) among household contacts, by WHO region, 2023
Indonesia is included in the WHO Western Pacific Region.
Globally, the cascade of TB preventive care shows a big gap between the number of household contacts screened for TB disease and the number starting TPT (Fig. 3.10).
Fig. 3.10 Cascade of care for provision of TB preventive treatment (TPT) to household contacts of people newly diagnosed with bacteriologically confirmed pulmonary TB disease, 2023
3.3 People living with HIV
Globally, the annual number of people living with HIV who received TPT increased from fewer than 30 000 in 2005 to 3.0 million in 2019 (Fig. 3.11). Subsequently, reported numbers fell for 3 years and have since stabilized at around 2 million people per year (1.8 million in 2024). Possible reasons for the reductions between 2020 and 2022 include disruptions to health services caused by the COVID-19 pandemic and changes in data collection. In a few countries, achievement of full TPT coverage among people living with HIV already on ART may have reduced the number of individuals eligible for TPT, limiting enrolment on TPT to people initiating ART.
Six high TB/HIV burden countries, accounting for 43% of the estimated global number of people living with HIV who developed TB in 2024 collectively accounted for 1.2 million (67%) of the global total in 2024: India, Mozambique, Nigeria, South Africa, Zambia and Zimbabwe. Each of these countries provided TPT to more than 100 000 people living with HIV in 2024, as they did in 2023. At regional level, there was a sharp increase in the numbers of people provided with TPT in the WHO Eastern Mediterranean Region in 2024, reflecting data reported for Pakistan.
Between 2005 (the year following the publication of the first WHO policy guidance on collaborative TB/HIV activities) and the end of 2024, 20 million people living with HIV were initiated on TPT, equivalent to just under half of the 40.8 million people estimated to be living with HIV in 2024 (9, 10).
Among 73 countries that reported data, a median of 38% (IQR: 6.1–62%) of people living with HIV who were newly started on antiretroviral therapy (ART) received TPT in 2024.
Fig. 3.11 Provision of TB preventive treatment (TPT) to people living with HIV, globally and by WHO region, 2005–2024
Indonesia is included in the WHO Western Pacific Region for the whole time series.
In 38 countries that reported data, a median of 84% (IQR: 73–95%) of people living with HIV who started TPT in 2023 completed their treatment (Fig. 3.12).
Fig. 3.12 Completion of TB preventive treatment (TPT) among people living with HIV, by WHO region, 2023
Indonesia is included in the WHO Western Pacific Region.
3.4 Screening for TB disease in household contacts and other high-risk groups
Among 124 countries that reported the results of TB screening in household contacts in 2024, the overall yield of people with TB was 1.5% (median: 1.7%; IQR: 0.63–3.6%) (Fig. 3.13). This is slightly lower than what would be expected in household contacts of people with bacteriologically confirmed TB (11). The wide variation among countries probably reflects differences in the coverage of screening for eligible individuals, the diagnostic algorithms being used and the completeness of reporting.
Fig. 3.13 Percentage of household contacts diagnosed with TB disease among those screened, by WHO region, 2024
Indonesia is included in the WHO Western Pacific Region.
In 2024, 106 countries reported the number of people newly diagnosed with TB who were identified through provider-initiated screening efforts in high-risk groups such as contacts, people living with HIV, people in prisons and mining communities, and through facility-based screening of people with diabetes and other groups (Fig. 3.14). In these countries the overall proportion of people newly diagnosed with TB detected through screening was 15% (median: 12%; IQR: 4.4–28%), while in the 22 high TB burden countries amongst them the proportion was 14% (median: 16%; IQR: 7.8–39%).
In 2024, 56 out of 66 priority countries reported data about the availability of chest radiography for regular TB screening or active TB case-finding campaigns. Of those 56 countries, 34 (61%) reported the regular use of chest radiography – with or without computer-aided detection software – in 75% or more of administrative units in the country (median coverage for 56 countries: 97% of administrative units, IQR: 26–100%).
Fig. 3.14 Percentage of people newly diagnosed with TB (new and relapse cases) reported through TB screening efforts, 2024

3.5 Tests for TB infection
Tests for TB infection can help to target TPT to people who can gain the most benefit from it. In 2024, 103 countries reported using tuberculin skin tests (TST) or interferon gamma release assays (IGRA) in either the public or private sectors to deliver TPT to populations at risk (Fig. 3.15). A further 12 countries reported using antigen-based skin tests in addition to IGRA or TST. Of the 33 countries reporting no use of tests for TB infection, 25 were in the WHO African Region.
Fig. 3.15 Diagnostic tests used for TB infection, by country, 2024

3.6 TB infection prevention and control
The risk of TB among health care workers relative to the risk in the general adult population is one of the indicators that WHO recommends for measuring the impact of TB infection prevention and control interventions in health care facilities. If effective prevention measures are in place, the risk ratio for TB in health care workers compared with the general adult population should be close to 1.
In 2024, 18 849 health care workers from 63 countries were reported to have been diagnosed with TB. The ratio of the TB notification rate among health care workers to the general adult population was greater than 1 in nine countries that reported five or more health care workers diagnosed with TB (Fig. 3.16).
Fig. 3.16 Notification rate ratio of TB among health care workers compared with the adult population, by country, 2024

3.7 Bacille Calmette-Guérin vaccination
Bacille Calmette-Guérin (BCG) vaccination is recommended as part of national childhood immunization programmes, in line with a country’s TB epidemiology (12). However, global coverage dropped from 89% in 2019 to 86% in 2020 and 85% in 2021, probably due to disruptions to health services caused by the COVID-19 pandemic. There was a recovery to 88% in 2022 and this level was also achieved in 2024 (Fig. 3.17) (13).
Fig. 3.17 BCG vaccination coverage in infants,a globally and by WHO region 2015–2023
References
The End TB strategy. Geneva: World Health Organization; 2015 (https://iris.who.int/handle/10665/331326).
WHA67.1: Global strategy and targets for tuberculosis prevention, care and control after 2015. Geneva: World Health Organization; 2014 (https://apps.who.int/gb/ebwha/pdf_files/WHA67-REC1/A67_2014_REC1-en.pdf#page=25).
WHO consolidated guidelines on tuberculosis. Module 1: Prevention – Tuberculosis preventive treatment, second edition. Geneva: World Health Organization; 2024 (https://iris.who.int/handle/10665/378536). License: CC BY-NC-SA 3.0 IGO.
WHO consolidated guidelines on tuberculosis. Module 2: Screening – Systematic screening for tuberculosis disease. Geneva: World Health Organization; 2021 (https://iris.who.int/handle/10665/340255). License: CC BY-NC-SA 3.0 IGO.
WHO guidelines on tuberculosis infection prevention and control. 2019 update. Geneva: World Health Organization; 2019. (https://iris.who.int/handle/10665/311259). License: CC BY-NC-SA 3.0 IGO.
WHO consolidated guidelines on tuberculosis. Module 6: tuberculosis and comorbidities, 2nd ed. Geneva: World Health Organization; 2025 (https://iris.who.int/handle/10665/382883). License: CC BY-NC-SA 3.0 IGO.
Bhargava A, Bhargava M, Meher A, Benedetti A, Velayutham B, Sai Teja G et al. Nutritional supplementation to prevent tuberculosis incidence in household contacts of patients with pulmonary tuberculosis in India (RATIONS): a field-based, open-label, cluster-randomised, controlled trial. The Lancet 2023;402:627–640. (https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(23)01231-X/)
Resolution 78/5: Political declaration of the high-level meeting of the General Assembly on the fight against tuberculosis. New York: United Nations; 2023 (https://undocs.org/A/RES/78/5).
UNAIDS epidemiological estimates, 2024 (https://aidsinfo.unaids.org/).
Interim policy collaborative TB/HIV activities. Geneva: World Health Organization; 2004 (https://iris.who.int/handle/10665/78705)
Fox GJ, Barry SE, Britton WJ, Marks GB. Contact investigation for tuberculosis: a systematic review and meta-analysis. European Respiratory Journal. 2013 Jan 1;41(1):140–56. (https://erj.ersjournals.com/content/41/1/140).
Weekly Epidemiological Record, 2018, vol. 93, 08, 73 - 96. Geneva: World Health Organization; 2018. (https://iris.who.int/handle/10665/260306).
The WHO Global Health Observatory (https://www.who.int/data/gho/data/indicators/indicator-details/GHO/bcg-immunization-coverage-among-1-year-olds-(-)). Data downloaded 21 July 2025.
General disclaimers
The designations employed
and the presentation of the material in this publication do not imply
the expression of any opinion whatsoever on the part of WHO concerning
the legal status of any country, territory, city or area or of its
authorities, or concerning the delimitation of its frontiers or
boundaries. Dotted and dashed lines on maps represent approximate border
lines for which there may not yet be full agreement.
