Nurse Akhter on duty in an inpatient area crowded with dengue patients at Suhrawardy Hospital in Sher-E-Bangla-Nagar, Dhaka, on 3 October 2023.
Emergency and critical care
Many proven health interventions are time dependent. Emergency care is an integrated platform for delivering accessible, quality and time-sensitive health care services for acute illness and injury across the life course. Integrated emergency care services facilitate timely recognition, treatment management and, when needed, continued treatment of the acutely ill at the appropriate level of the health system.
Critical care is an ongoing, intensive treatment provided to patients with life-threatening illnesses or injuries that require close, constant monitoring and support. Care is typically delivered in critical care units (e.g. intensive care units or high dependency units). Critically ill patients often need advanced medical equipment and therapies, intravenous medications to support heart function or blood pressure, and continuous monitoring of vital signs.
Over half of deaths and over a third of disability in low- and middle-income countries could be addressed by the implementation of effective emergency and critical care. Prioritizing an integrated approach to early recognition, resuscitation, treatment and prevention of complications from acute conditions reduces the morbidity and mortality from a wide range of diseases across the life course.
The recent pandemic has revealed pervasive gaps in the provision of emergency and critical care and reinforced the need for an integrated approach to these services. Emergency and critical care are pivotal service delivery platforms of health systems, and have an essential role in saving lives, reducing disabilities, and preventing complications.
Especially when there are logistical or financial barriers to healthcare access, people may present for care only when symptomatic with acute illness or injury. Emergency care is powerfully aligned with the primary health care agenda as it provides first contact clinical care for those who are acutely ill or injured. Pre-hospital and facility-based emergency care is a high impact and cost-effective form of secondary prevention. Ongoing critical care ensures adequate monitoring, reassessment and continuing comprehensive treatment to maximize patient outcomes.
Emergency and critical care play an important role in public health. Disease surveillance at facilities delivering emergency and critical care is essential to guide primary prevention and outbreak response. Building capacity for emergency and critical care is the vital foundation for the health systems ability to surge during larger scale health emergencies such as conflict, natural disaster or outbreaks of epidemic disease.
The Seventy-sixth World Health Assembly called on WHO to prioritize integrated emergency, critical and operative care for universal health coverage (UHC) and protection from health emergencies (WHA 76.2). WHO is dedicated to assisting countries to strengthen their emergency and critical care systems to ensure quality everyday clinical care and robust responses during times of crisis. Through collaborative efforts and partnerships, WHO advocates for the integration of emergency and critical care into national healthcare agendas, emphasizing the importance of building national capacities to enhance clinical service readiness, preparedness and resilience. This includes working closely with partner agencies within the UN system to ensure that emergency and critical care are appropriately represented in UHC packages and planning and disaster readiness and response.
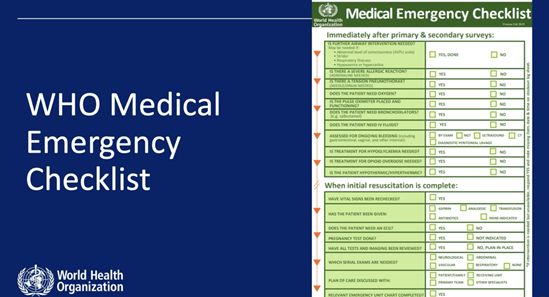
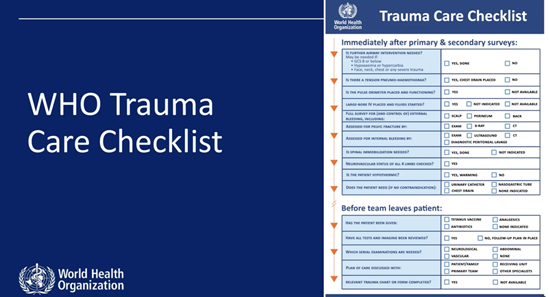
WHO’s work plan on emergency and critical care encompasses various facets, including advocacy, policy and planning, assessment at system level and health facility level, clinical learning programmes, clinical process tools and improvement of clinical care. WHO's Clinical Services and System Unit is dedicated to strengthening health systems to deliver emergency and critical care, particularly in first contact locations, and to supporting the development of quality, timely emergency and critical care accessible to all.